It is an autosomal recessive syndrome:
- Insufficient cortisol syntesis
- Increased ACTH production –> increases cortisol to maintain circulating levels
- Stress cortisol – inadequate
- Mineralocorticoid synthesis affected
- 21 beta-hydroxylase deficiency & 17 alpha-hydroxylase deficiency for steroid hormone production
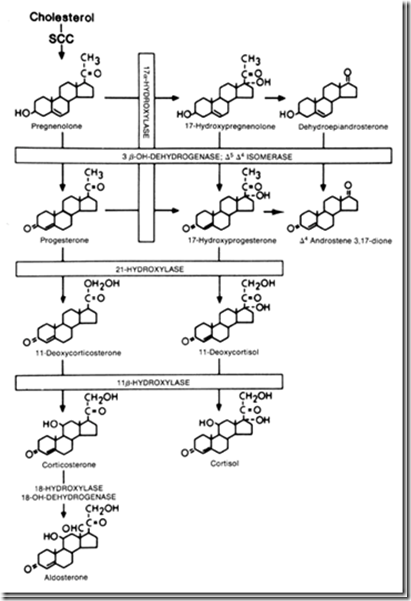
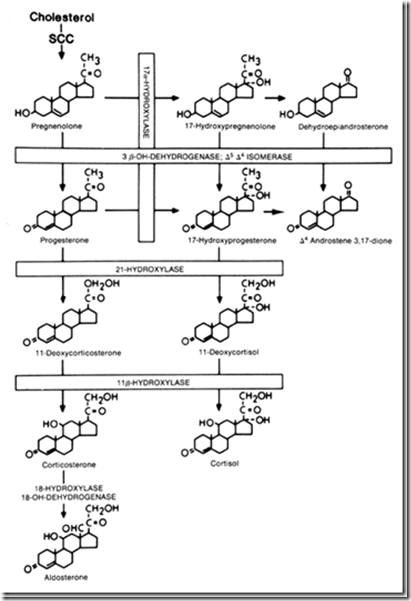
21 beta-hydroxylase deficiency: (refer diagram)
- Coding gene at chromosome 8
- Mineralocorticoid defect results in hyperkalemia, hyponatremia & low aldosterone level
Defect in:
- unable to convert progesterone –> 11-deoxycorticosterone
- unable to convert 17-hydroxy progesterone –> 11-deoxycortisol
Therefore, there will be increase in:
- adrenal androgens (testosterone)
- DHEA
- androstenedione
- ACTH
As the body pushes the adrenal gland harder to correct the low cortisol level (compensation), in return, more testosterone is made instead.
Hyperandrogenism
- Increased risk of fertility
- Accelerated growth
- Precocious puberty (excessive prepubertal androgens)
- Hirsutism
- Irregular menstrual cycles
Treatment
- Correcting the levels of cortisol with substitute therapy so that body will recognise normal levels of cortisol and stop trying to produce excessive amounts of cortisol (which will end up with excessive testosterone)
17 alpha-hydroxylase deficiency (refer diagram):
Defect in:
- Impaired 17-hydroxyprogesterone synthesis
- Impaired 17-hydroxypregnenolone synthesis
- Impaired cortisol synthesis
- Impaired androgen synthesis
Will manifest:
- Hypertension
- Hypokalemia
- metabolic alkalosis
Hypertension inhibits renin secretion –> decreased angiotensin 2 –> decreased aldosterone.
11-hydroxylase deficiency
Increase in:
- Deoxycorticosterone production
Elevated deoxycorticosterone suppresses effect of aldosterone.
Will manifest: (less aldosterone effect)
- virilization
- hypertension
- hypokalemia
Conclusion
There will be decrease in:
- aldosterone
- cortisol
And increase in:
- testosterone
- DHEA-s