Recap of the previous post :
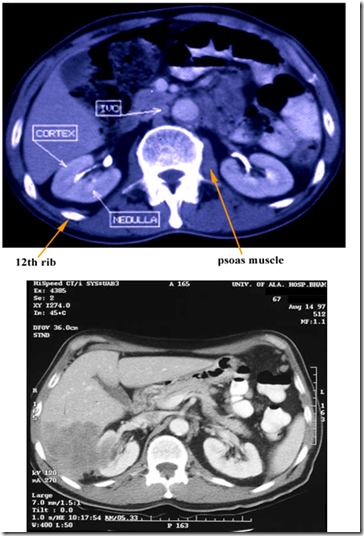
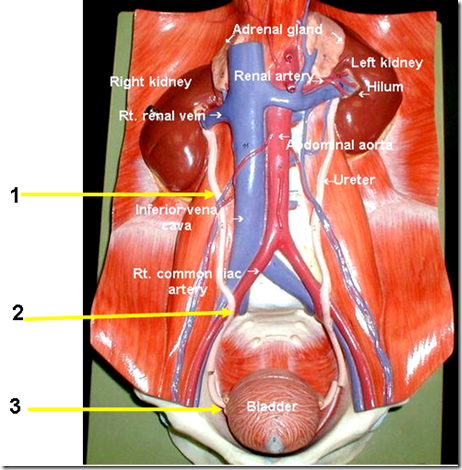
- Location of the kidney
- coverings of the kidney
- muscles that are clinically related (quadratus lumborum etc)
- transpyloric plane – hilum
- differentiate kidney/splenic swelling (refer clinical notes)
- histology
- PCT, DCT –> difference in microscopic structure
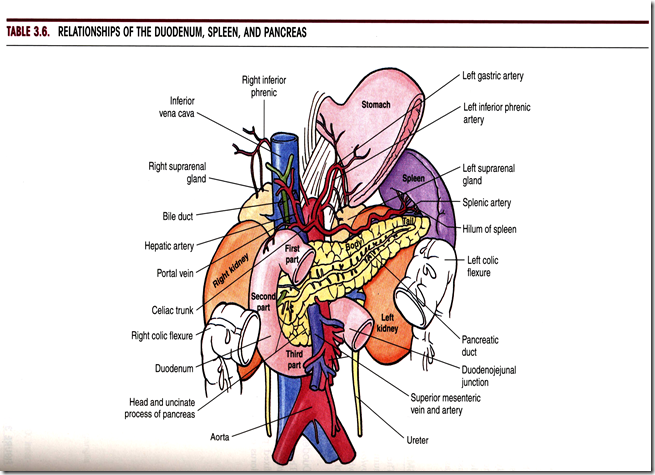
Surgical relations
Left kidney
- Behind stomach lesser sac
- Infront left kidney : pancreas, splenic artery, stomach
- Left renal vein also drains left gonadal vein
Right kidney
- next to pouch of morrison (most dependent area for pus collection)
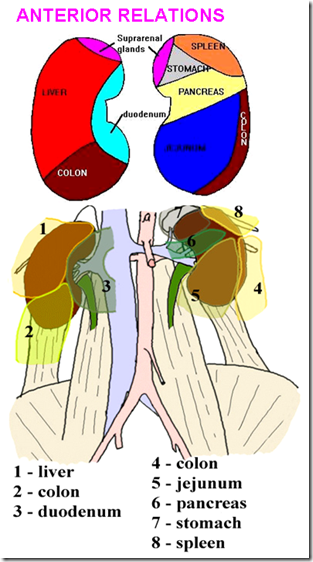
Anterior relations
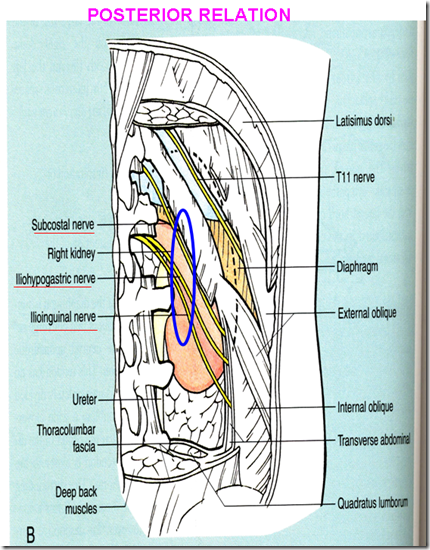
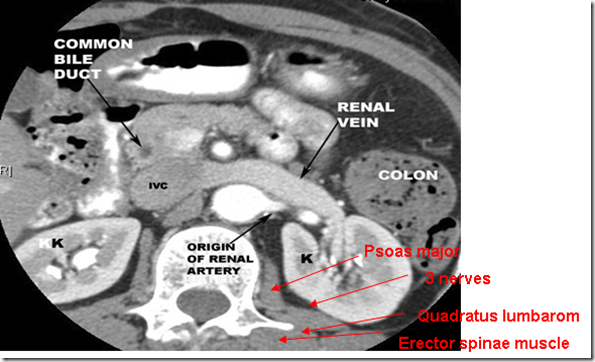
Posterior Relations
3 important nerves lying anterior to the kidney:
- subcostal nerve
- iliohypogastric nerve
- nephrectomy: post operative anaesthesia over the root of the scrotum –> nerve affected is the iliohypogastric nerve
- ilioinguinal nerve
Renal plexus
Sympathetic
- Abdominopelvic splanchnic nerves
- Have pain fibers
- Spinal segments: T11- L2 (loin pain – small of the back)
- Supplies the skin as well
Parasympathetic
- Vagus nerves
- No pain fibers
Nerves to Ureter:
- Renal plexus
- Aortic plexus
- Superior hypogastric plexus
Renal colic:
- very severe pain
- presenting suddenly and without warning
- at upper lateral mid back over the costovertebral angle (renal angle)
- radiates inferiorly and anteriorly towards the groin
- Usually caused by stones in the kidey, renal pelvis or ureter
- Pain is caused by dilatation, stretching & spasm of the ureter
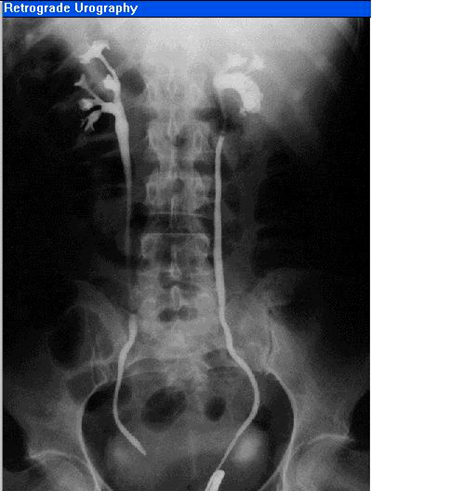
Retrograde urography
From external urethral meatus, inject dye into the ureteric meatus. It is not invasive, therefore no pressure over kidney
Intravenous Pyelogram
Radio opaque dye. If kidney is not functioning properly, do not inject radio opaque dye, it will give more pressure to kidney. Only good to observe a normal kidney. Therefore it is not as preferable as the Retrograde Urography for diagnostic purposes.
Surface anatomy of the ureter in radiology can be found:
- lying on psoas major & tranverse processes (over the lumbar verterbra)
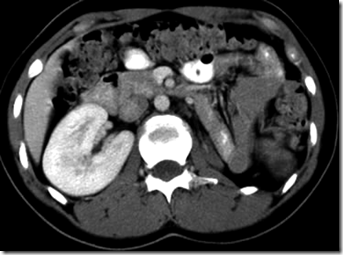
CT Scanning
Left side: liver & right kidney
Right side: pancrease & left kidney
________________________________________________________________
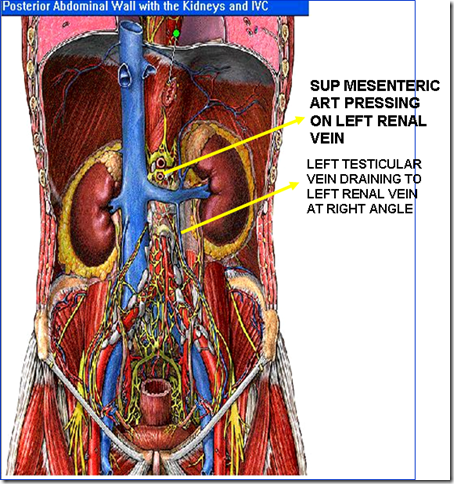
Left renal vein:
Also drains left testicular vein at right angle.
- Left kidney
- Left suprarenal
- Left testes, left ovary (left gonads)
Right renal vein:
Drains:
- Right kidney
- Right suprarenal
The left testes appears to be larger than the right testes. It is due to the left sided varicocele due to pressure effect on the left renal vein by the superior mesenteric artery. The superior mesenteric artery will obstruct the left renal vein, therefore will be ineffective drainage of blood in the left testicular vein causing a collection of blood in the left testis. The testicular vein will be dilated causing left sided varicocele.
The ureter
Q: In xray, where are the 3 areas that we can see radio-opaque shadow? (the constrictions)
- where renal pelvis joins abdominal part of ureter
- where it crosses pelvic brim
It enters pelvis by crossing bifurcation of common iliac arteries infront of sacro-iliac join.
- where it pierces the urinary bladder
Ureter:
-
25 cm long
- 3 parts
1) Pelvis of ureter
From hilum to lower pole of ki
dney
2) Abdominal part
From inlet of pelvis/pelvic brim to lateral angle of urinary bladder
3) Pelvic part, has 3 parts:
- From inlet of pelvis to ischial spine
- From ischial spine to outer wall of urinary bladder
- This part passes obliquely through bladder wall for about 2cm until opens into lateral angle of internal trigone
Course:
- Runs vertically downwards behind parietal peritoneum
- on psoas major muscle
IN FEMALE
In female:
- runs forward through the broad ligament (ligaments that connects uterus to lateral pelvic wall)
- related closely to cervix of uterus & uterine artery
- Also forms floor of ovarian fossa
Clinical significance:
When clamping uterine artery for surgery, ureter can be clamped accidentally.
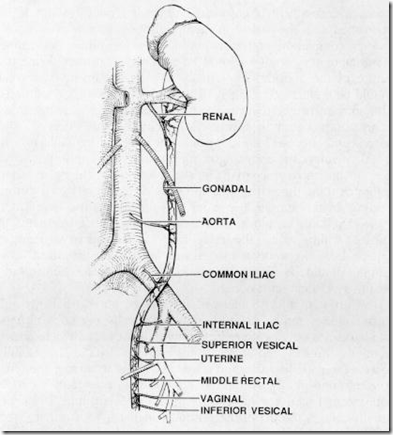
Blood supply of the ureter:
Ureter receives blood supply from:
- Renal artery
- Aorta
- Common iliac artery
- Internal iliac artery
- Superior vesical artery
- Inferior vesical artery
In female, extra 2: (chain of anastomosis)
- uterine
- vaginal
During surgery, stripping of arteries can damage ureteric wall, because ureter depends on blood supply to undergo peristalsis for the excretion of urine. Therefore in this case, flow of urine can also be disrupted and might be the result of ureteric stricture.
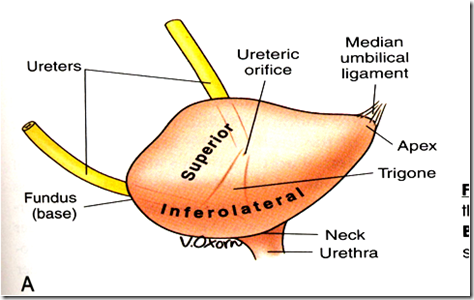
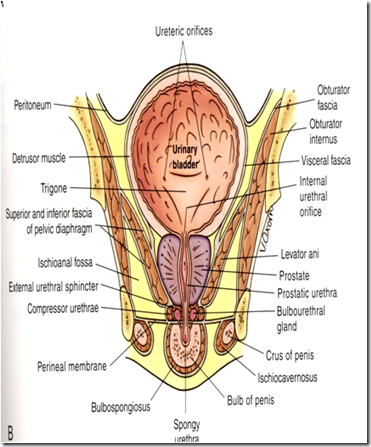
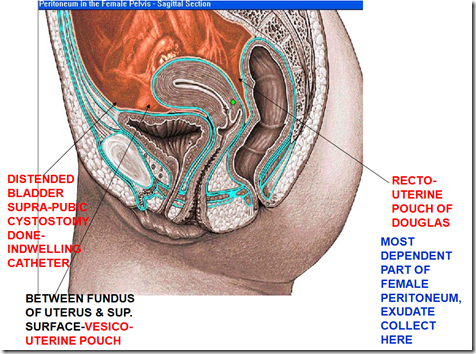
_____________________________________________________________________Urinary Bladder
In young child:
- above pelvis
In adult:
- empty bladder –> lies in pelvic cavity behind pubic bones
- Urinary bladder full (500ml) –> part of bladder lies in lower abdomen (hypogastric region)
Parts of urinary bladder:
- Apex
- Base (posterior surface)
- Neck
- Superior surface
- Inferolateral surface
Blood supply:
- Superior vesical artery
- Inferior vesical artery
Venous drainage:
- Vesical venous plexus
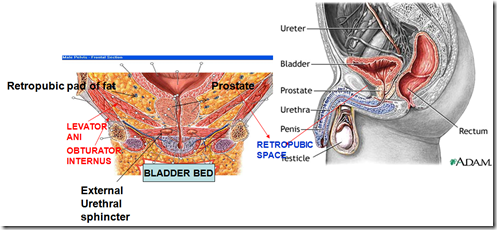
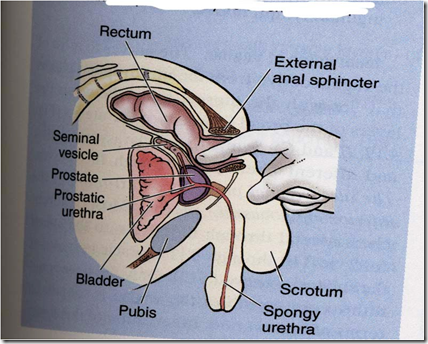
Insertion of catheter will be resisted by 3 parts (curvature):
- At the bend of the penis (lift it up to straighten it)
- External urethral sphincter (voluntary – painful!)
- Internal urethral sphincter (involuntary)
If patient is unable to urinate for 24 hours (probably due to ureteric stones), there will be retention of urine in the urinary bladder. Urinary bladder will be distended into the abdominal cavity (full bladder). Therefore, perform a suprapubic cystostomy, the urine will flow out through there. This is like catheterisation but at the suprapubic region.
What are the structures in the bladder bed?
- Retropubic pad of fat
- Levator ani
- Prostate
- External urethral sphincter
Internal Trigone of bladder
Internal trigone: Equilateral triangle on inner aspect of bladder.
Entire bladder wall consists of many mucous folds, but there are no folds over the internal trigone (tense mucosa).
At the apex lies the: (inferior)
- Internal urethral orifice
At the base: (superior)
- Ureteric ridge
Internal urethral sphincter : Circular smooth muscle (involuntary)
Compressor urethrae/sphincter urethrae/external urethral sphincter (around membranous urethra): Actual voluntary sphincter (voluntary, control flow of urine)
When the integrity of the internal urethral sphincter is compromised –> incontinence.
Nerve supply of the urinary bladder
Autonomic
Parasympathetic (S2-4)
- Pelvic Splanchnic nerve
- ganglia on bladder wall
- contraction of detrusor muscle –> micturition reflex
- autonomic reflex
Sympathetic (T11-L2)
- Hypogastric plexus
- postganglionic fibres run in hypogastric plexus
- Beta receptor: relaxes bladder wall
- Alpha receptor: control internal urethral sphincter during filling (tonicity)
- Incontinence: lack of sympathetic tone
Somatic
Pudendal nerve (S2-4)
- supply voluntary external urethral sphincter
Q: What are the 3 areas of the CNS that is involved in micturition?
1) Sacral Micturition centre (S2-4)
- Bladder contraction (stretch internal trigone –> sympathetic) by detrusor muscle (parasympathetic)
2) Pontine Micturition centre
- Relaxation of external sphincter (v
oluntary)
3) Cerebral cortex (paracentral lobule)
- Inhibit sacral centre
Q: Injury of the sacral nerve root (S2-4) will cause:
- Detrusor areflexia
- Inability of detrusor muscle to contact
- Bladder will not be able to contract even when it is filled up
- Bladder will be distended
- Internal urethral sphincter will not be able to hold the large amount of urine –> overflow incontinence
_____________________________________________________________________
Urethra
Difference between male & female urethra
Female:
- Urethra: 4cm
- Embedded in anterior wall of vagina
- Orifice infront of vaginal orifice –> more chances of infection
Male:
- Urethra: 20cm
- 3 parts: Prostatic, membranous & penile (spongy)
- Penile part have 2 curves
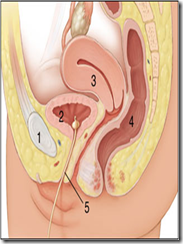
Structures at posterior surface of urinary bladder in MALE:
Structures inside prostate:
- vas deferens
- seminal vesicle
- ejaculatory duct (vas deferens & seminal vesicle join)
Prostatic utricle: a blind sac, where numerous prostatic glands opens into prostatic urethra.
Secretions (for the protection of sperm):
- Acidic neutralize alkalinity of vaginal secretion
- Acid phosphatase
- Prostaglandin
- Zince
_____________________________________________________________________
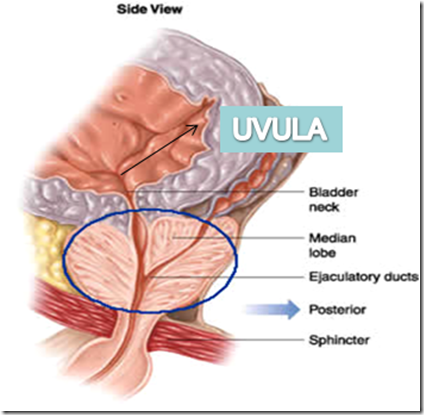
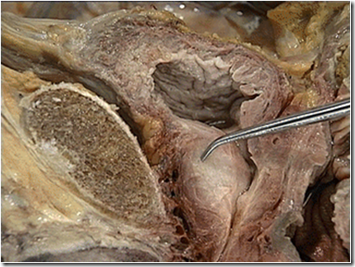
Prostate
Prostate is a fibro-muscular-glandular organ, surrounding neck of urinary bladder & prostatic urethra.
Parts of prostate:
- Apex
- rests on sphincter urethrae
- Base
- around neck, anterior, posterior & infero-lateral surface
Lobes: (5)
- Anterior
- Median lobe
- In between 2 ejaculatory duct & prostatic utricle on back & urethra anteriorly
- 2 lateral lobes
- Posterior lobe
Q: Benign prostate hypertrophy (BPH): enlargement of inner part of gland, most MEDIAN lobe, by the action of TESTOSTERONE. Swelling of the uvula –> compresses the internal urethral orifce -> intermittent retention of urine. This occurs mostly in aged man, where there is always a frequent urge to urinate, however, urine cannot be expelled.
In BPH, transurethral approach (thru urethra) and enucleation of swelling is done.
True capsule of the prostate:
- Connective tissue of the prostatic gland
False capsule of the prostate:
- Outer to the true capsule: pelvic fascia
- It is in between veins of prostate.
- Therefore, if surgery is done from external, there will be bleeding. So, transurethral approach is favourable.
Structures inside the prostate:
- Vas Deferens
- Seminal vesicle
- Ejaculatory duct
- Multiple prostatic gland (acidic –> protect sperm)
- Prostatic utricle
- Prostatic urethra
Prostate can be felt par-rectal, during rectal examination.
Clinically important relations of the female urinary system.












>good atricle!
very good illustration of anatomy!!!
Please is there any university you will advise me to join and do my clinicals? Am currently in my third year school of medicine Ahfad university Sudan. Thank you