*Read from printed notes – Ian Brown
_____________________________________________________________________
Notes from emedicine.com
Background
- Brain tumors may originate from neural elements within the brain, or they may represent spread of distant cancers.
- Primary brain tumors arise from CNS tissue
- account for roughly half of all cases of intracranial neoplasms
- The remainder of brain neoplasms are caused by metastatic lesions.
- In adults, two thirds of primary brain tumors arise from
- structures above the tentorium (supratentorial)
- In children, two thirds of brain tumors arise from structures below the tentorium (infratentorial).
- 95% of brain tumours
- Gliomas
- Low grade
- Astrocytoma
- common in young people
- High grade
- Anaplastic astrocytoma
- Gliobastoma multiforme
- metastases
- meningioma
- pituitary adenoma
- acoustic neuroma
- Classification by tumor cell type is irrelevant to the emergency physician because emergent treatment is the same regardless of the tumor type.
Pathophysiology
- Tumors of the brain produce neurologic manifestations through a number of mechanisms
- Small, strategically located tumors may damage specific neural pathways traversing the brain
- Tumors can invade, infiltrate, and supplant normal parenchymal tissue, disrupting normal function.
- Because the brain dwells in the relatively restricted repository of the cranial vault, growth of intracranial tumors with accompanying edema may compress normal tissue and impair function
- Space-ocupying lesion
- May manifest vision problems, and headaches
- Tumors proximal to the third and fourth ventricles
- may obstruct the flow of cerebrospinal fluid
- leading to hydrocephalus
- In addition, tumors generate new blood vessels (ie, angiogenesis)
- disrupting the normal blood-brain barrier
- causing edema
- The cumulative effects of tumor invasion, edema, and hydrocephalus may elevate the intracranial pressure (ICP)
- impair cerebral perfusion
- Intracranial compartmental rise in ICP may provoke shifting or herniation of tissue
- under the falx cerebri
- through the tentorium cerebelli OR
- through the foramen magnum
- Slow-growing tumors
- particularly tumors expanding in the so-called silent areas of the brain
- such as the frontal lobe
- may be associated with a more insidious course
- These tumors tend to be larger at detection
- Most primary brain tumors do not metastasize
- Of those neural element tumors that do
- intraparenchymal metastasis generally precedes distant hematogenous dissemination via the arterial system
- Metastatic brain tumors from non-CNS primary tumors may be the first sign of malignancy
- or they may herald a relapse.
- Nonetheless, the signs and symptoms of brain metastases simulate those of primary brain tumours
Diagnosis
History
- headache
- altered mental status
- memory loss and decreased alertness
- suspect: frontal lobe tumour
- depersonalization, emotional changes, and behavioral disturbances
- Temporal lobe neoplasms
- increased irritability, unsteadiness, ataxia, headache, vomiting, and progressive obtundation
- paedetric posterior fossa tumour
- ataxia
- nausea & vomiting
- weakness & gait disturbance
- Sensory disturbance
- vision
- smell
- hearing
- intermittent (then progressive) hearing loss, disequilibrium, and tinnitus
- acoustic neuroma
- focal seizures, fixed visual changes, speech deficits, or focused sensory abnormalities
- onset of symptoms usually is insidious, but an acute episode may occur with
- bleeding into the tumor, or
- when an intraventricular tumor suddenly occludes the third ventricle
- seizures, hemiparesis, visual field cuts, speech difficulties, and intellectual disturbance.
- Supratentorial tumors in children
- Pituitary adenoma
- Non-functional
- when large enough can compress optic chiasma
- causing vision problems
- Hypersecretory
- secrete prolactin
- women
- amenorrhea-galactorrhea syndrome
- men
- impotence
Physical examination
- Increased Intracranial pressure
- papillaedema
- Diplopia
- compression/displacement of 6th CN
- at base of brain
- Impaired upward gaze (Parinaud syndrome)
- may occur with pineal tumours
- Homonymous hemianopia
- tumour of occipital lobe
- Anosmia
- frontal lobe tumours
- Brainstem and cerebellar tumors
- cranial nerve palsies
- ataxia
- incoordination
- nystagmus
- pyramidal signs
- sensory deficits
- Facial, cochlear, and vestibular CN dysfunction
- run through the cerebellopontine angle
- Vestibular nerve
- acoustic neuroma
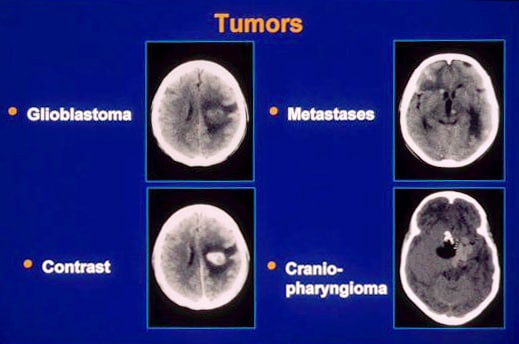
Imaging studies
- CT
- Intravenous contrast
- for tumour idenfication
- May appear
- hypodense
- isodense
- hyperdense
- MRI
- helpful in identifying
- tumours in posterior fossa
- including acoustic neuroma
- haemorrhagic lesions
- Xray
- tumour on sella turcica
- pituitary tumour/adenoma
- Lumbar puncture
- not needed
Complications
- Acute hemorrhage into a tumor
- Brain neoplasms predisposed to hemorrhage include lung cancer, melanoma, and choriocarcinoma.
- Lesions near the third ventricle can cause
- paroxysmal symptoms of headache, syncope, or mental status change.
- vomiting, ataxia, memory changes, visual disturbances, or personality change
s may occur - Episodic increases in ICP
- secondary to pressure arising from blockage of cerebrospinal fluid outflow
- Sudden death
- obstruction of outflow drainage from the third ventricle
- Sudden increases in ICP
- may lead to life-threatening brain herniation
- shifts the brain parenchyma in the direction of least resistance:
- caudally through the foramen magnum (posterior fossa tumors) or
- transtentorial apertures.
- Some pituitary tumors are hormonally active
- acromegaly
- galactorrhea
Treatment
Prehospital Care
- Supportive
- Airway disturbance
- breathing difficulty
- Signs of pronounced elevation in ICP
- Impairment of consciousness
- May necessitate definitive airway control with endotracheal intubation
- Hyperventilation.
Emergency Department Care
- Corticosteroids
- may dramatically reduce signs and symptoms related to cerebral edema
- experience relief within the first few hours of steroid therapy
- Dexamethasone
- agent of choice
- minimal salt-retaining properties
- For patients with signs or symptoms of impending herniation and airway compromise
- consider use of adjunctive medications for rapid sequence intubation
- These might include lidocaine and medication for rapid-onset neuromuscular blockade, with precautions to diminish fasciculations
- Induction agents, such as thiopental, may be used
- After definitive control of the airway,
- consider gentle hyperventilation
- Mannitol
- Hyperosmolar agent
- Reduce ICP & cerebral oedema
- creating an osmotic gradient across an intact blood-brain barrier
- between cerebrospinal fluid in arachnoid space and blood plasma
- May have rebound
- Increases in ICP
- makes its use problematic
Surgical intervention/Radiotherapy
- Tumour resection/debulking
- Installation of ventricular shunt
- Placement of radioactive implants

I would like to know more about neoplastic lesions of the brain