Pheochromocytoma
- Also known as: paraganglioma, chromaffinoma
- Intra-adrenal sympathetic paraganglioma
- Sporadic lesions: tend to be unilateral
- Familial lesions: tend to be bilateral
- 1.4-18% are incidentalomas
- Co-exist with extra-adrenal paragangliomas (can also occur outside adrenal medulla)
Pheochromocytoma associated genetic syndromes:
- Multiple Endocrine Neoplasia (MEN) type 2
- Von-Hippel-Lindau (VHL) syndrome
- Neurofibromatosis (NF) type 1
- Hereditary paraganglioma (PGL) syndromes – mitochondrial complex 2 gene
Pheochromocytomas may be the initial manifestation of these genetic syndromes.
Clinical features:
LION model (catecholamine excess)
- palpitations
- hypertension –> throbbing headaches
- anxiety
- chest pain
- abdominal pain
- sweat
- breathlessness
- 2ndary diabetes mellitus
Spells (episodes): variable, spontaneuous or precipitated by postural changes, anxiety, exercise, or increased abdominal pressure.
Macroscopic:
- 3-5cm (may be up to 10cm)
- Encapsulated
- Cut surface: gray/white –> tan (on exposure to air)
- Focal hemorrhage
- Degenerative changes
- Cystic
- Calcification
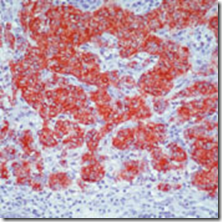
Microcopic:
- Alveolar (zellballen) / trabecular architecture / mixture
- Pseudocapsule
- Tumour cells resemble normal chromaffin cells
- Cytoplasm: granular, basophilic/amphophilic
- Nuclear & cytological pleomorphism (no prognostic significance)
Immunohistochemistry:
Chromogranin A +ve in all neuroendocrine tumours (not only in pheochromocytoma)
Synaptophysin +ve (neural origin)
Criteria for malignancy:
- Presence of METASTASIS
- If there is metastases, catecholamine excess is more obvious
_____________________________________________________________________
Extradrenal Paraganglioma
Pheochromocytoma occuring outside of the adrenal medulla, in ectopic sites.
- Anywhere along parasympathetic/sympathetic chain
- Histologically identical to the ones in adrenal medulla
- Names by anatomical site
- Common: Carotid body , jugulotypanic (chemodectoma), vagal paraganglioma
- Only 1% clinically functioning
- Potato tumour