Summary of thyroid tumour:
Usually tumours seen are primary epithelial tumours. Adenomas are benign & carcinomas are malignant.
Classification
By it’s histogenic/differention properties:
- Exhibiting follicular cell differentiation (95%)
- Exhibiting C-cell differentition
- Exhibiting follocular & C-cell differentiation
Types of thyroid tumours
Epithelial tumours
- follicular adenoma (most common)
- papillary adenoma
- Hurthle cell (oncocytic) tumours
- hyperfunctioning follicular cell
- Undifferentiated carcinoma
- Anaplastic
- Sarcomatoid
- Medullary carcinoma
- Others:
- Follicular carcinoma
- Clear cell tumours
- Squamous cell/mucinous
- Poorly differentiated carcinoma (insular carcinoma)
- C-cell hyperplasia
- Other neuroendocrine lesions
Lymphoid tumours & tumour-like conditions
- Malignant lymphoma
- Plasmacytoma
- Hodgkin’s disease
- Langerhans’ cell granulomatosis
- Rosai-Dorfman disease
Mesenchymal tumours
- Benign
- lipoma
- hemangioma
- lymphangioma
- leiomyoma
- neurilemoma
- solitary fibrous tumour
- Sarcoma
- fibrosarcoma
- liposarcoma
- leipmyosarcoma
- chondrosarcoma
- osteosarcoma
- malignant schwannoma
- angiosarcoma
Other primary tumors & tumour-like conditions
- Teratomas
- Infants/Children: cystic/benign
- Adults: Malignant
- Parathyroid tumours
- problems of diff diagnosis?
- Amyloidosis
- systemic disease/localised primary amyloid tumour
- Malakoplakia
- Extramedullary hematopoiesis
- associated with myelofibrosis
Metastatic tumours
- Direct extension
- Blood-borne metastasis
_____________________________________________________________________
Follicular adenoma
Definition:
Benign encapsulated tumour with follicular cell differentiation
- solitary
- surrounded completely by a thin capsul
- compressed gland
*haemorrhagic, well-encapsulated
Microscopic patterns (not important)
- normofollicular (simple)
- macrofollicular (colloid)
- microfollicular (fetal)
- trabecular/solid (embryonal)
- papillary
Secondary degenerations
- Hemorrhage
- Oedema
- Fibrosis
- Calcification
- Bone formation (ossification)
- Cystic degeneration
Differential diagnosis
- Dominant nodule of nodular hyperplasia
- clinical
- Minimally invasive follicular carcinoma
- gross
- Follicular variant of papillary carcinoma
- microscopic
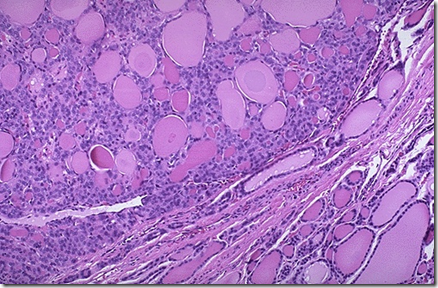
Note the well defined capsule.
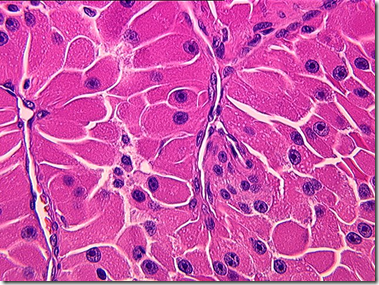
Hurthle cell adenoma: a variant of follicular adenoma.
Note the distinct nuclueses of the Hurthle cells.
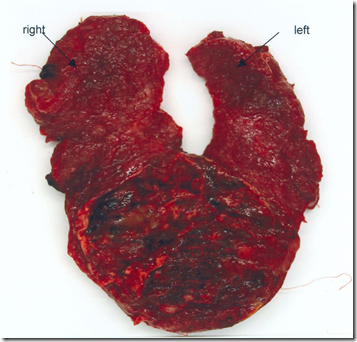
Follicular carcinoma
- Rare neoplasm
- Woman, 30 years old, whites
- Invasion of capsule, blood vessels / adjacent thyroid
Types
- Minimally invasive
- Widely invasive
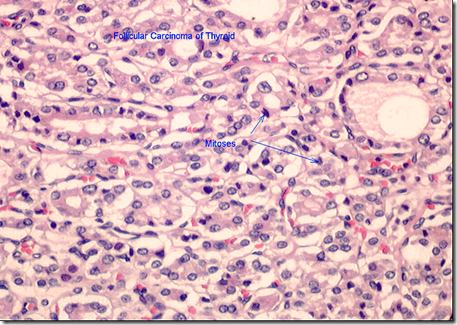
Microscopy
- Well-formed follicles
- Poorly-formed follicles
- Cribiform area
- Trabecular formations
- Predominantly solid growth pattern
- Cytoplasmic clear changes
- Mitotic activity & nuclear atypia
Diagnosis
- Immunohistochemistry
- **Epithelial membrane antigen (EMA)
- thyroglobulin
- low molecular weight keratin
- basement menbrane components (laminin & type IV collagen)
- ras point mutation (53%)
_____________________________________________________________________
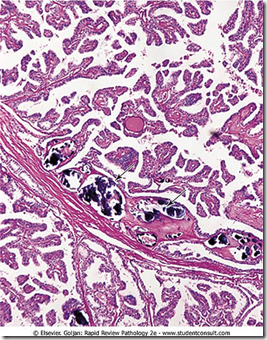
Papillary carcinoma
Image: Gross papillary formation with central fibrosis
- Follicular carcinoma: most common neoplasia
- Papillary carcinoma: most common malignancy
- Female, 40 years old
- 90% thyroid malignancies in children
Gross feature:
- Variable size
- Solid, whitish, firm, clearly invasive
- Less than 10% surrounded by a complete capsule
- Marked cystic changes (10%)
- Papillary formations evident to naked eye (finger-like projections)
Microscopy
1. Architectural features:
- True papillae
- Complex, branching & randomly oriented
- Central fibrovascular core
- Single/stratified lining of cuboidal cells
2. ***Nuclear features:
Image: Orphan Annie Eyes
- Orphan Annie eyes
- Ground glass nuclei (optically clear)
- Nuclear pseudoinclusions
- Nuclear grooves
- Nuclear microfilaments
3. Psammoma bodies
Image: Laminated calcification, also seen in benign tumours & goiter
Diagnosis
- Immunohistochemistry (not important, easily diagnose microscopically)
- Keratin
- Thyroglobulin
- S-100 protein
- EMA, CEA, Vimentin, Ceruloplastin
- Estrogen receptor proteins
- Oncogene alterations
- RET & NTRK1 (tyrosine kinase ativity)
- Activation of N-ras (point mutation)
Alot of morphologic variants, but nuclear features are seen in all.
Prognosis depends on
- Females better prognosis
- More than 40 yo
- Extrathyroid extensions
- History of previous irradiation
- Tumour size
- Capsule & Margins
- Multicentricity**
- Distant metastasis**
- Poorly differentiated, squamous, or anaplastic foci
- EMA & LeuMI positivity (good prognosis)
- DNA ploidy
_____________________________________________________________________
Medullary carcinoma
Also known as
- solid carcinoma
- hyaline carcinoma
- C-cell carcinoma
No capsule and composed of parafollicular C-cells
Gross:
- solid, firm & non-encapsulated
- but well circumscribed
- Continuous fibrous capsule (rare)
- Located in the midportion of upper half of the gland
- Corresponding to a greater concentration of C-cells
Microscopy:
- *Amyloid (stain +ve)
- Solid proliferation
- Round to polygonal cells
- Granular amphophilic cytoplasm
- Medium sized nucleus
- Highly vascular stroma
- Hyalinized collagen
- Coarse calcification
Amyloid: stained with congo red birefringence
Diagnosis
- Ultrastructurally
- cytoplasmic dense-core variably sized secretory granules
- Immunohistochemistry
- *Calcitonin (+ve)
- Keratin
- NSE
- Chromogranin A, B & C
- Synaptophysin
- Opioid peptides
- CEA
- **Negative for thyroglobulin
- distinguishes from other thyroid cancer
_____________________________________________________________
Anaplastic carcinoma
- Elderly
- Rapidly growing mass
- **Hoarseness, dysphagia & dypsnea
- Extrathyroid extentions (most)
Gross
- highly necrotic
- hemorrhagic
- solid tumour mass
Microscopic (not important)
- Cellular variants
- Squamoid
- Spindle clee
- Giant cell
- *Paucicellular
- 1. Neutrophilic infiltration
- 2. Prominent vascularization
- 3. Cartilaginous/osseous metaplasia
- Patterns of growth
- Fascicular
- Storiform
- Palisading at the necrotic edges
Diagnosis
- Ultrastructural
- Epithelial differentiation
- Immunohistochemistry
- Keratin
- Vimentin (Spindle cell)
- Laminin
- 390 & focal EMA & ECA (Basement membrane)
_____________________________________________________________________
Thyroid lymphoma
- Primary malignant lymphoma
- adult/elderly
- females
- Rapid enlargment
- tracheal & laryngeal compression
- dyspnoea, hoarseness
- Euthyroid (mostly)
- Sometimes hypothyroid
Gross
- Cut surface
- Solid white with fish flesh appearance
Microscopic
- Mostly diffuse large cell type
- Sclerosis (focally prominent)
- Immunoblastic lymphoma
- Low grade lymphomas
- small/intermediate cells
- Diffuse / follicular pattern
- Packing of follicular lumina of lymphoma
Diagnosis
- Immunohistochemistry
- leukocyte common antigen
- B-cell markers
Hodgkin’s disease of the thyroid gland (lymphoma)
Note: Reed-sternberg cell
_____________________________________________________________________
Angiosarcoma of the thyroid
Tumour is well-differentiated & composed of anastomosing vascular channels lined by epithelioid endothelial cells.
_____________________________________________________________________
Staging of cancer
Staging of well-differentiated thyroid cancers is related to age for Stage 1 & 2. But not for Stage 3 & 4.
Younger than 45 years old
- Stage 1
- T – any
- N – any
- Stage 2
- T -any
- N- any
- M1
Older th
an 45 years old
- Stage 1
- T1 (less than 1.5cm)
- Stage 2
- T2-3 (more than 1.5cm)
- Stage 3
- T4 NO
- TO N1 (spread to outside thyroid by not outside neck)
- Stage 4
- T – any
- N – any
- M1
Factors favouring malignancy
- Age
- Males
- Neck irradiation in infancy
- Solitary nodules (more likely to be malignant)
- Rate of growth
- Ipsilateral adenopathy (1 sided)
- Toxic/got nodules (less likely to be malignant)
- Cystic nodules (less likely to be malignant than solid ones)
MRI is better than CT for the evaluation of metastatic, retrotracheal or mediastinal lesions
Serum thyroglobulin levels is useful in monitoring patients after removal of a papillary/follicular carcinoma.