Important things to cover
- Gross anatomy of the kidney
- Surface anatomy
- Parts
- Clinically important relations
- Coverings of kidney
- Structures at sagittal section of kidney
- Blood supply of kidney
- Microscopic structure of the kidney
- Gross & microscopic structure of the ureter, urinary bladder & urethra
Histology is important (look for atlas of histology)
_____________________________________________________________________________________________
Basic anatomy of the renal system (read up foundation 1)
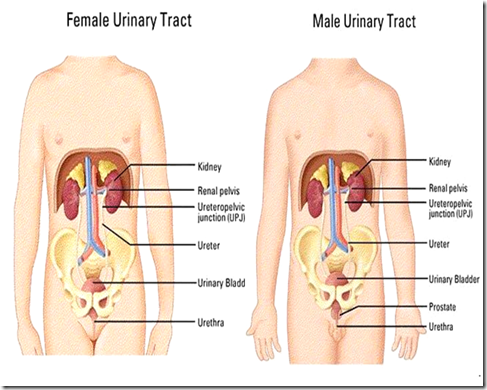
The urinary system consists of:
- 2 kidneys
- Excretory passages
- Major & minor calyces
- Ureters
- Urinary bladder
- Urethra
What are the major differences in male & female?
Female:
- Pelvic part of ureter
- close relation to cervix of uterus
- Clinical importance: During surgery relating to the cervix, the blood supply of the kidney might be accidentally clamped. The peristalsis of the urethra is dependant on it’s blood supply, so if it’s deprived, urine cannot be excreted.
- It is susceptible to infection (Urinary tract infection)
- urethra short
- no subdivisions
Male:
- urethra longer
- have subdisivions, divided into 3 parts
- prostatic
- membranous
- penile
- Urinary passage: genito-urinary (also expels semen)
The kidney
- 1700ml of blood filtered everyday
- 1.3 million nephrons in each kidney
- Removes:
- toxic by-products of metabolism (as urine)
- conserve salts
- conserve water
- reabsorb glucose & proteins
- Regulate blood pressure, haemodynamics & acid-base balance
- Endocrine function: produce renin, erythropoietin & prostaglandin
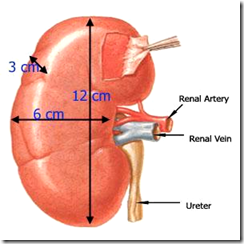
The gross kidney is:
- reddish brown (due to it’s abundant blood supply
- bean shaped
- upper pole bend medially
- left kidney longer & narrower
- kidneys move down 1 inch on inspiration
- about 150gm
- 12L/6W/3T (cm)
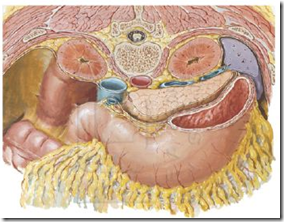
- located behind peritoneal cavity
- on posterior abdominal wall
- either side of vertebral column
This is a CT scan at the coronal section. Each time reading a CT scanning diagram, always remember that it’s opposite in sides, the left side is actually the right side. Therefore, looking at the left kidney in the diagram is actually the right kidney in reality.
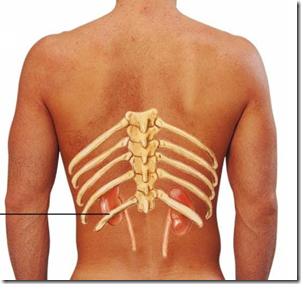
Notice that the left kidney is higher (highest border T11 lowest border L2) whereas the right kidney is lower (highest border T12 lowest border L3). The right kidney is less enclosed by the rib cage, because of the presence of right lobe of liver above it, therefore pushing it down. So, the right kidney is palpable during inspiration (moves down by 1 inch).
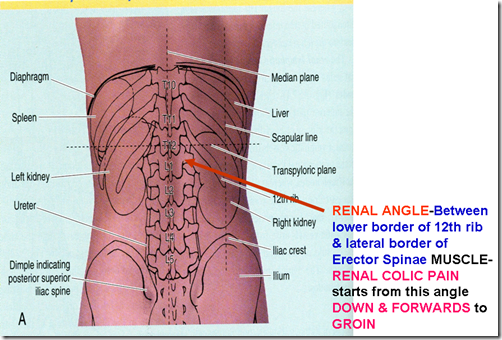
The renal angle as seen in the image, is located between the
- lower border of the 12th rib
- & lateral border of the erector spinae muscle
Therefore, renal colic pain starts from this angle down & forward to the groin (LOIN TO GROIN PAIN)
Left kidney related to 11th & 12th rib. Right kidney related to only 12th rib.
The right kidney is covered by both the pleura (above the 12th rib) and diaphragm (below the 12th rib), therefore extra care is taken when inserting any sharps on the right kidney, because if the pleura if punctured, pneumothorax can take place.
The hilum of the kidney correlated to the transpyloric plane (midway bwtn suprasternal notch & upper margin of symphysis pubis)
* Q: What is metabolic acidosis?
*Q: If BP drops/anemia/hypovolaemic, kidney will shutdown. How?
Anatomy of the kidney
- upper pole – thick & round
- lower pole – conical
- anterior surface – convex
- posterior surface – flat
- lateral margin – convex
- medial margin – concave & thicker
Hilum: middle-depressed area. Structures at hilum (anterior-posterior): VAP
- Renal Vein
- Renal Artery
- Pelvis of Ureter
- Additional: accessory artery & vein pass behind ureter. + lymphatic, nerves & fats.
Renal sinus: Fat filled extension of hilum deep inside kidney substance.
Suprarenal:
- Right suprarenal – pyramidal & over upper pole
- Left suprarenal – crescentic, comma shaped & over upper part of medial margin
Note the:
- renal hilum
- renal s
inus
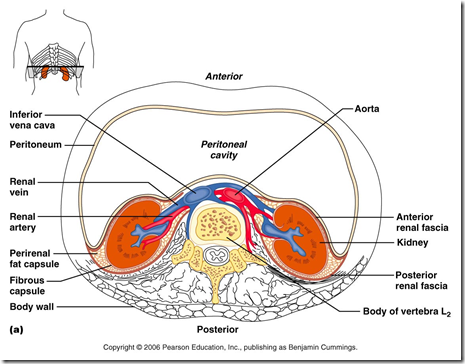
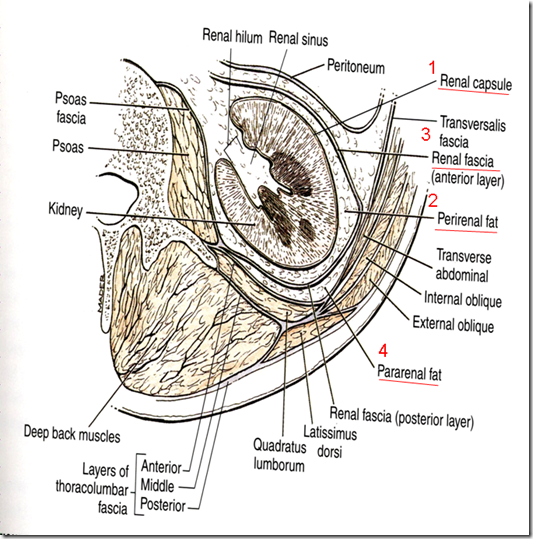
Coverings of the kidney (supports): (in – out)
1) Renal fibrous capsule
2) Perirenal fat (fatty capsule)
- posterior part of kidney
3) Renal fascia (false capsule/fascia of gerota) –
- from post abdominal wall
- Connective tissue continuous with fascia transversalis
- fused with suprarenal (natural barrier of infection)
- renal fascia goes infront of post abdominal wall & continue to opposite kidney, infection can travel across the connective tissue & adrenal gland.(paranephritis?)
4) Pararenal fat
- Surrounding renal fascia & posterior to it
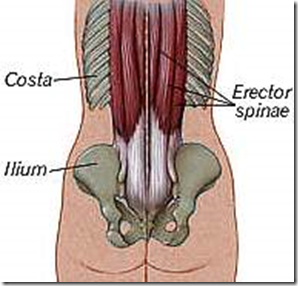
Surgical exposure of kidney
From the back:
- Skin
- Superficial fascia
- Posterior layer
- Thoracolumbar fascia
- Erector spinae muscle
- Middle layer
- Thoracolumbar fascia
- Quadratus lumborum muscle
- Anterior layer
- Thoracolumbar fascia
- Coverings of kidney
Between the anterior layer & kidney lies 3 nerves supplying the anterior abdominal wall (image). Therefore, take extreme care not to damage the 3 nerves during renal surgery, or patient will return with parasthesia of the anterior abdominal wall.
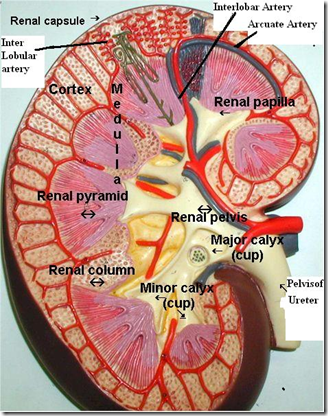
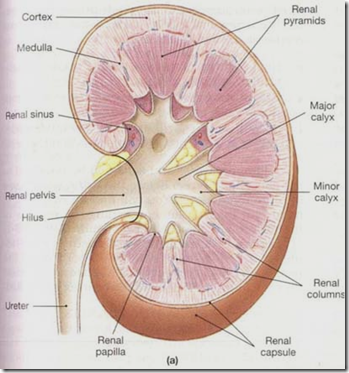
Sagittal section of the kidney
3 regions:
- Pelvis of ureter
- 3 major calyces
- 8-18 minor calyces
- Medulla
- 8-18 pale triangular pyramids (contain straight part of nephron: LOH & Collecting duct)
- Cortex
- Outer cortical region
- Inner juxtamedullary region ( contains nephrons – convoluted part)
Renal column: Column of Bertin – lies between the renal pyramids
Lobe of kidney: A renal pyramid (with associated cortical arch)
Renal papilla: Apex of renal pyramid – towards medial (pierced by 18-20 ducts of bellini)
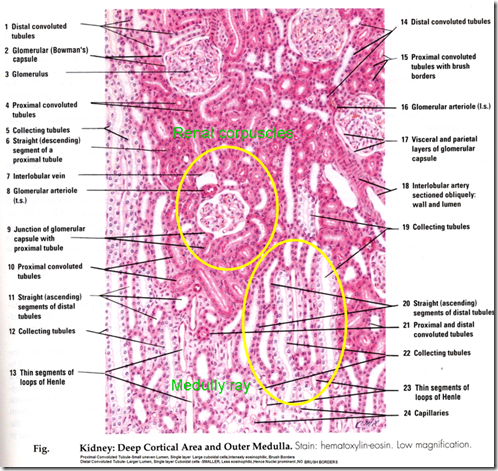
In Cortex : Contains
- Renal Corpuscles (glomerulus + bowman’s capsule)
- Convoluted tubules (labyrinth)
- Long striated medullary rays (corticol continuation of straight part of nephron, LOH, CD)
In Lobule of kidney
- Each medullary ray with part of cortex surrounding.
*Q: How do you identify renal cortex in a histologic section?
- Renal corpuscles (multiple)
- Convoluted tubules/labyrinth (PCT, DCT)
- Medullary ray (continuation of straight part, produce ray like appearance, LOH, CD)
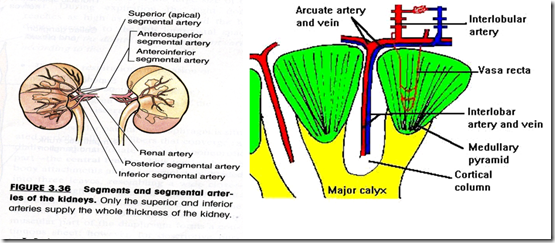
Blood supply (recheck with Foundation 1)
- Renal artery
- 5 segmental branch
- interlobar branch (btwn pyramids)
- interlobular branch
- afferent arteriole
- glomerulus
- efferent arteriole to:
1) cortical glomeruli –> form peritubular network (reabsorption ard PCT)
- interlobular vein
- arcuate vein
2) juxtamedullary glomeruli –> form vasa recta
- venulae recta
- arcuate vein
- interlobular vein
- lobar vein
- renal vein
The urine is able to flow from base to apex because of the countercurrent mechanism( btwn vasa recta & LOH?), maintaining the osmolality.
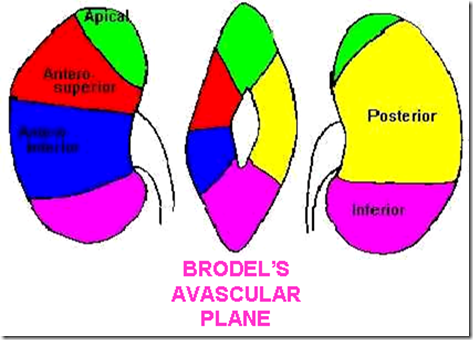
There are 5 area supplied by the arteries:
- Apical
- antero-superior
- Antero-inferior
- posterior
- inferior
The only place that is not supplied is the hilum, therefore incision starts here to prevent massive blood loss.
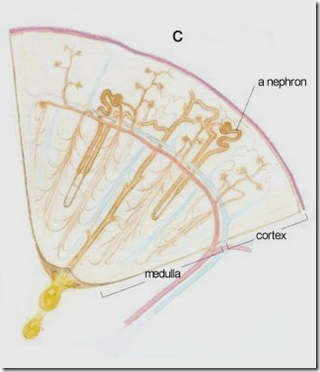
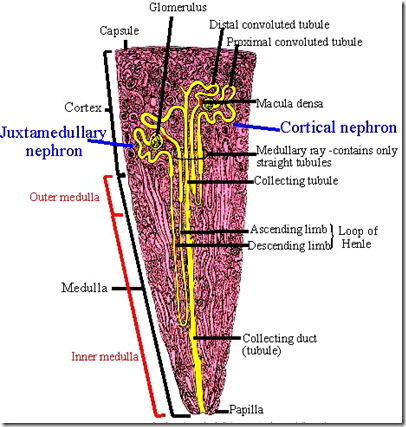
This is the image of 1 nephron. The functional unit of a kidney is:
- Nephron + Collecting tubule = uriniferous tubule
Parts of a nephron:
- Bowman’s capsule
- PCT (Pars convoluta & pars recta) – Descending LOH
- LOH
- DCT(Pars convoluta & pars recta) – Ascending LOH
- Multiple nephrons open into a collecting duct
- multiple collecting ducts join to form large duct of bellini, which perforate papilla.
2 types of nephrons:
- cortical (85%)
- short LOH
- juxtamedullary (15%)
- long LOH extending to pyramids
Straight part of nephron runs in the pyramid.
_____________________________________________________________________________________________
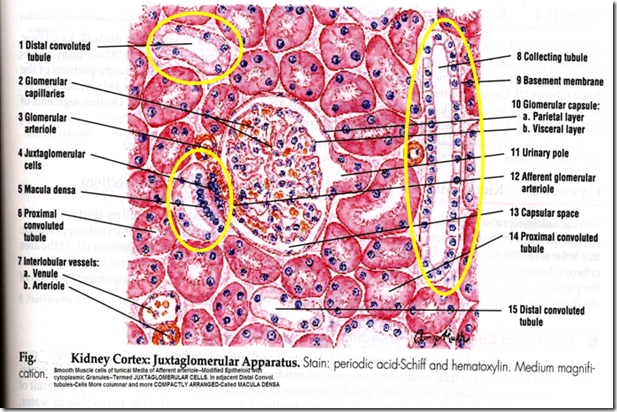
MICROSCOPIC STRUCTURE OF THE KIDNEY (IMPORTANT)
H&E stain
- Renal corpuscles
- 200-250 micro dia
- oval structure
- glomerulus & bowman’s capsule
- 2 poles: vascular & urinary pole
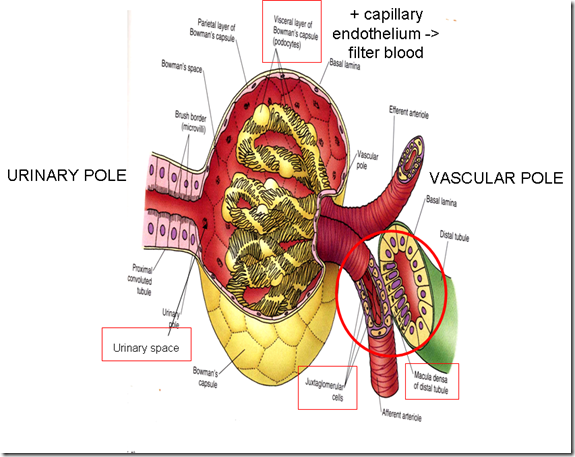
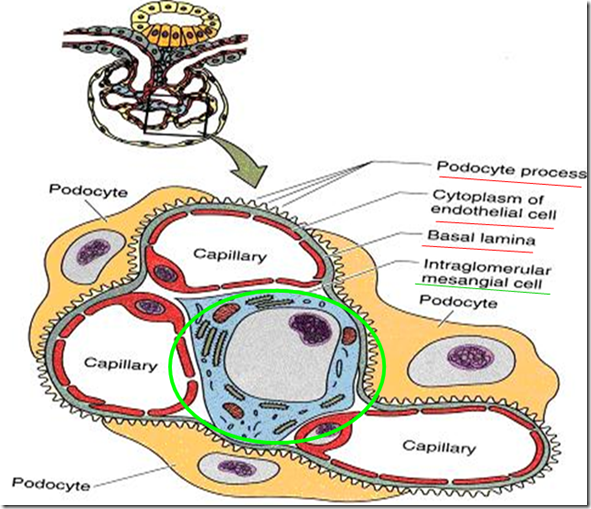
Bowman’s capsule has 2 layers:
- Inner Visceral layer
- Modified epithelial cells with tentacle like processes called podocytes – filtration slits between pedicels
- Outer Parietal layer
- Simple squamous epithelium on a thin basement membrane (No function)
The space between these 2 layers is called: urinary space.
The visceral layer of the Bowman’s Capsule/podocytes + capillary endothelium are responsible in filtering the blood.
Note the:
- Juxtaglomerular cells (does not look like a arteriole)
- Macula densa (does not look like a convoluted tubule)
The filtration barrier
The filtration barrier consists on 3 structural parts: (85% of filtration)
1) Capillary endothelium
- Have fenestrations between endothelial cells
2) Podocytes
- Have slits
3) Combined basal lamina (MAIN STRUCTURE FOR FILTRATION BARRIER
- basal lamina of endothelium
- basal lamina of podocytes
If the basal lamina is deformed, filtration is ineffective, albumin & RBC will be able to pass through –> microalbuminuria & hematuria. This is the hallmark of nephropathy.
Basal lamina have 3 layers:
- Middle lamina densa
- type IV collagen
- Do not allow albumin + RBC to pass
- Lamina Rarae on each side (2)
- Laminin
- Fibronectin
- Heparan sulphate
- Polyanionic protein
Q: What is the main mechanism by which basal lamina act? (prevent filtration of protein, RBC, Macromolecules)
1) Mechanical barrier
- lamina densa
2) Electrical/charge barrier
- lamina rarae
- contains polyanionic protein that charges albumin. Albumin will not be able to pass thru, the basal lamina is –ve charge, albumin is now –ve charge.
In Diabetic patients, basal lamina thickens –> proteinuria.
Mesangial cells (15% of filtration)
It is the special cells formed by connective tissue of afferent arteriole. They maintain the integrity of the basal lamina by phagocytosis
_____________________________________________________________________________________________
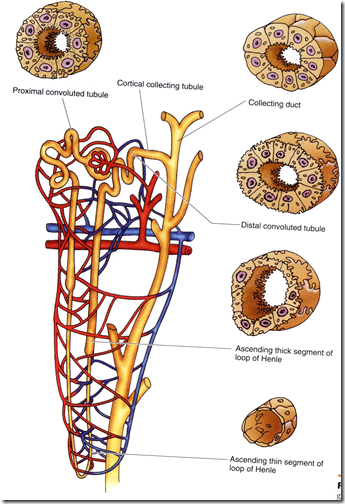
Proximal Convoluted Tubule (TUBULAR REABSORPTION)
- 14mm long
- 60micro Diameter
- Lined by single layer simple cuboidal epithelium
- intense pink eosinophilic granular cytoplasm
- well developed brush border/microvilli
- lumen small & uneven (occluded by microvilli)
- Microvilli increase surface area & accomodate protein channels (required for maximum tubular reabsorption)
- Cells have alot of mitochrondria & basal infoldings
Distal Convoluted Tubule (ACTIVE SECRETION OF K+ & H+)
- 4-5mm long
- 45micro diameter
- Lined by single layer low cuboidal epitelium
- Pale cytoplasm
- No microvilli
- Wide lumen
- Cells narrow
- Nucleus more prominent
Aldosterone acts on DCT: Increase Na reabsorption (Acid-base balance) –> Increase blood volume
_____________________________________________________________________________________________
RENAL MEDULLA
Thin Limb of Loop of Henle
- Lined by Simple Squamous epithelium
- Descending limb
- Permeable to water
- Ascending limb
- Less permeable to water
Countercurrent multiplier system: Produce hypertonic urine
Collecting Duct
- Not part of nephron
- 20mm long
- Lined by single layer simple cuboidal epithelium
- Pale cytoplasm
- some cells are intercalated
- cell membranes are very visible
ADH acts on CD: Increase water channels (aquarporins) –> increase water reabsorption
Papillary Duct
- terminal part of collecting duct
- wide lumen
- lined by pale staining columnar epithelium
Straight part of PCT & DCT
- Similar to epithelium of PCT & DCT in cortex
_________________________________________________________________________________
Juxtaglomerular apparatus
- Near the vascular pole of the glomerulus
- afferent arteriole & DCT are in close contact
- they develop structural changes producing juxtaglomerular apparatus
- JA maintains hydration of patient
JA consists of 3 components:
- Juxtaglomerular cells (JG cells)
- Tunica media of the afferent arteriole ->
- Smooth muscles get epitheliod changes ->
- Round nucleus with cytoplasm granules (precursor of RENIN)
- Macula Densa
- The DCT coming in contact with JG cells –>
- Basement membrane disappear
- cells become columnar
- densely packed & prominent nucleus
- senses the urine in DCT (not blood)
- La
cis cells (Polkissen cells)- clusters of polyhedral cells
- between vascular pole & distal tubule
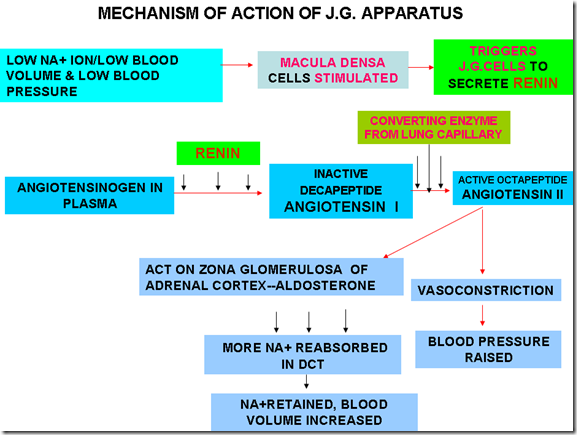
Mechanism of action of JG apparatus:
- Stimulus
- Low Na+
- Macula Densa stimulated (urinary ionic changes, not blood)
- Low BV, Low BP
- JG cells stimulated
- Low Na+
- Triggers JG cells –> secrete renin
- Renin converts angiotensinogen to angiotensin 1
- Angiotensin 1 reaches lung endothelium
- Angiotensin converting enzyme converts angiotensin 1 to angiotensin 2
- Angiotensin 2 acts on
- Zona glomerulosa of adrenal cortex – secrete aldosterone –> reabsorb Na+ in DCT –> increase BV
- Vasoconstriction –> BP raised
_____________________________________________________________________________________________
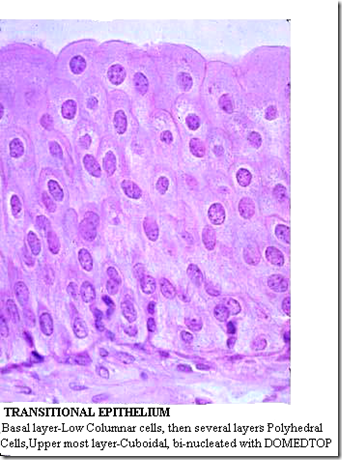
Transitional Epithelium
It is found in the parts of the kidney that acts as carriage apparatus, because it provides a protective coat. This transitional epithelium is found in:
- urinary bladder
- ureter
- major calyx & minor calyx
- upper part of urethra
Features of transitional epithelium:
- surface cells (umbrella shaped)
- sometimes bi-nucleated
- eosinophilic glycoprotein coat (impermeable to urine)
- connected to one another by desmosomes
- so that they maintain position when stretched/relaxed
- desmosomes contract –> umbrella cells flatter –> prevent damage from high pressure of urine
- surface cells alter thickness during distension –> bear pressure of urine
_____________________________________________________________________________________________
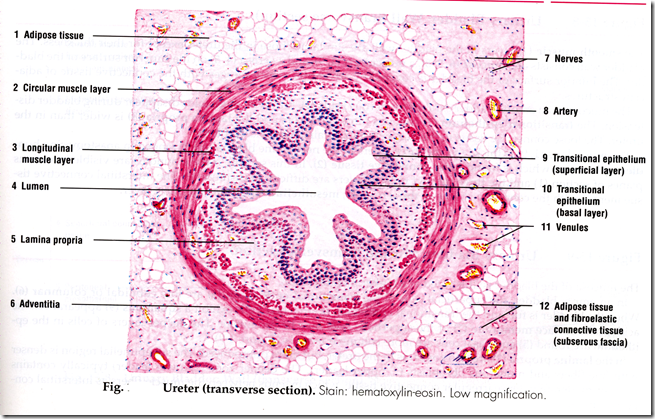
Microscopic structure of ureter
*Note that the lumen is star-shaped.
Consists of 4 coats: (out to in)
- Adventitia coat (fibrous)
- Muscular coat (Smooth muscle) – opposite from GIT (produce peristalsis)
- Outer circular
- Inner longitudinal
- Lamina propria
- Mucous membrane
- Transitional epithelium
- multiple folds – star shaped lumen
_____________________________________________________________________________________________
Microscopic structure of the Urinary Bladder
Layers:
1) Outer adventitia coat
2) Muscular coat
- Smooth muscles (Detrusor muscles) arranged in:
- Inner longitudinal
- Middle circular
- Outer longitudinal
- Circular layer at neck forms: internal urethral sphincter (involuntary)
3) Lamina Propria
4) Mucosa
- Transitional epithelium
- Folds: 6-8 layer thick






oooh!!! this site is super. i got what i wanted. keep it up. i have only gotten world class help from http://www.funbiology.com i never knew i will come a superb site like it again.thanks
Thanks!
I found this very helpful. Awesome site.
Thanks
fantastic site
interesting
this is a good way to raised You knowledge , so good site
Your publication is quite consumable, buton your work i did not see any referenceses. I need it to do some comparesm
thank you for this article, i found it pretty good. Only negative thing I could list is the quality of the pictures.