Brief info on calcium:
- Calcium is important for many physiologic processes
- Neurons are very sensitive with changes in Ca2+ ion concentration
- 0.1%: in ECF
- 1%: in cells
- 98.9%: stored in bones & teeth
- Most abundant cation in the body
- Calcium in plasma is present in 3 forms:
- protein bound form (can’t diffuse capillary membrane)
- ionized form (can diffuse capillary membrane)
- physiologically active
- complex form (complex with anions)
Functions of calcium
- Structural integrity & metabolism of bone
- bone growth & remodelling
- tooth formation
- Synaptic transmission
- presynaptic ending, calcium enters –> neurotransmitter exits
- Control of excitability of nerve & muscle cells
- stabilization of membrane potentials
- by modulation of permeability to Na+ & K+
- Excitation-contraction coupling in muscle
- exocytosis for endocrine & exocrine glands)
- Coenzyme function
- haemostatis & complement systems (blood clotting)
- Regulation of transmembrane ion transport
- Bidirectional calcium transport
- in ER, sarcoplasmic reticulum, mitochondria
- Cell motibility
- 2nd messenger in intracellular signal transduction pathways
Calcium homeostasis
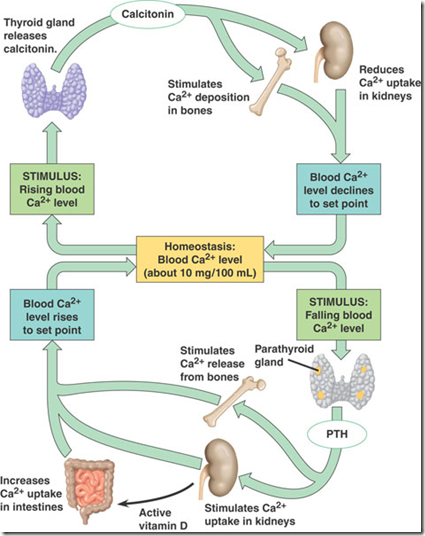
This is a summarised representation of calcium homeostasis.
An increase in Ca2+ in blood, Calcitonin will be secreted from parathyroid gland and stimulate
- Ca2+ deposition in bone (storage)
- Ca2+ reabsorption in kidney decreases
A decrease in Ca2+ in blood, PTH will be secreted from parathyroid gland and stimulate
- Ca2+ release by bone
- Ca2+ reabsortion in kidney increases
- Kidney releases active Vitamin D
- Increases Ca2+ uptake in intestine
_____________________________________________________________
Calcium regulation involves
- 3 tissues
- bone
- intestine
- kidney
- 3 hormones
- Parathyroid
- calcitonin
- activated Vit D3
- 3 cells
- osteoblasts
- osteocytes
- osteroclasts
Regulation of calcium
- Intestinal absorption (vit D dependent)
- duodenum
- proximal jejunum
- Renal tubular reabsorption & excretion
- Exchange of calcium between plasma & bone
- bone remodelling
Calcium absorption
Calcium absorption occurs in the small intestine by
- Active transport
- Duodenum & proximal jejunum
- Diffusion
- Ileum
Once absorbed, intracellular transport involves carrier proteins, intestinal calcium-binding protein & cytosolic calcium-binding protein.
Active transport
Across the basolateral membrane
- Mg2+ – Ca2+ – ATPase
- Primary active transport
- Ca2+/NA+ exchanger
- Secondary active transport
Vitamin D3/Calcitriol/1,25 dihydroxyvitamin D3
- regulates amount of cytosolic calcium binding protein
- activates the active transport systems
Parathyroid hormone
- increases small intestinal absorption
- by enhancing 25-OH D-1 hydroxylase activity & calcitriol synthesis
Renal excretion
- 10% ingested calcium will be excreted in the urine
- Ionized & complex forms only can be filtered in the glomerulus
- 70% reabsorbed in proximal tubule
- transcelluar absorption via calcium channels (down electrochemical gradient)
- calcium extrusion across basolateral membrane/active transport (against electrochemical gradient)
- Paracellular absorption
- across tight junctions (Between epithelial cells)
- 20% reabsorbed in the LOH
- 9% reabsorbed in he distal tubule
- transcellular absorption through voltage sensitive Ca2+ channels (activated by PTH)
- 1% excreted in urine
_____________________________________________________________________
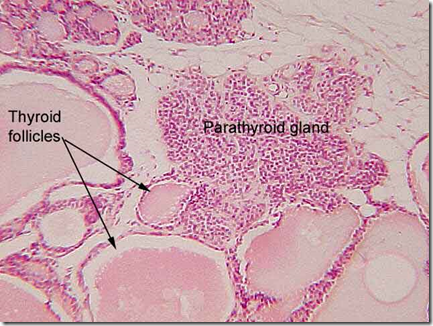
The parathyroid glands & it’s hormones
- 4 parathyroid glands
- 2 superior 2 inferior
- behind the thyroid gland
- macroscopic appearance: dark drown fat
- removal of 2 parathyroid glands will not cause any abnormalities, but removal of 3 or more will cause transient hypoparathyroidism
- Cells
- Chief cells: secrete most of the PTH
- Oxyphil cells
Parathyroid hormone
- Maintains the plasma ionized calcium level
- calcium sensing receptor are located on the parathyroid cell surface
- detects the serum calcium concentration & determine the set point for the serum PTH concentration
- Mg2+ required for PTH release & to perform it’s effects on target tissues
- PTH binds to plasma membrane G-protein coupled receptors on target cells (bone & kidney)
- PTH levels follow a diurnal circadian pattern
Structure
- Biological activity confined to the NH2-terminal 34 amino acid sequence
- no disulphide linkages
- Encoded on chromosone 11
- Circulating half life : 2-4 minutes only
Bone cells
- osteoblast: bone formation
- osteoclast: bone resorption/ breakdown
Actions of PTH
- Bone
- releases Ca2+ from bone
- Bone resorption
- Direct effect of osteroblasts which then stimulates osteocla
sts - transports calcium from bone to ECF (increase in serum calcium level)
- phases
- Rapid phase: begins in minutes and increases progressively for several hours, results from activation of already existing bone cells (osteocytes) to promote calcium & phosphate absorption
- osteoblasts & osteocytes have receptors for PTH
- PTH stimulate calcium pump at the bone fluid side of the osteocytic membrane
- calcium pump transfers calcium ions into the ECF
- Slower phase: several days/ weeks to become fully developed. Results from proliferation of osteoclasts, followed by greatly increased osteoclastic reabsorption of the bone
- Activation of osteoclasts by PTH
- Activation of osteoblasts & osteocytes send 2ndary signals to osteoclasts for bone resorpsion
- Osteoclastic osteolysis
- increased osteoclastic size & no.
- increased osteoclastic collagenase & lysosomal enzyme activity
- increased osteoclastic acid phosphatase, carbonic anhydrase, lactic acid, and citric acid concentration
- increased bone resorption
- mobilization of Ca+, Mg2+ and inorganic phosphate
- Increased osteoblastic number
- also has bone formation effect, but less than resorptive effect
- Increased collagen synthesis
- for osteoid
- Increased alkaline phosphatase activity
- for resorption process
- Increase local growth factors
- IGF & transforming factors
- GIT
- Increase calcium uptake
- Acts synergistically with vit D
- indirect action thru vitamin D (induce a calcium-binding protein in the duodenal & jejunal mucosa)
- Increase absorption of phosphate
- Acts synergistically with vit D
- Kidney
- Increase reabsorption of calcium
- Increase urinary excretion of phosphate
- Reduces tubular reabsorption of phosphate
- Formation of Vit D3
- acts on intestine
- Decrease Na+ and bicarbonate reabsorption from the proximal tubule
Calcitonin
- effects opposite to PTH (decrease plasma calcium concentration)
- from parafollicular cells/C cells
- Effect of calcitonin in children is much greater
Actions of calcitonin
- Decrease absorptive activities of the osteoclasts & osteolysis
- Deposition of calcium in the bone salts
- Prolong & decrease formation of new osteoclasts
- minor effect on kidney
- excretion of calcium, natrium & phosphate
- inhibit tubular reabsorption
- decrease synthesis of vit D3
- by inhibiting renal 1 alpha-hydroxylase activity
- Inhibit gastric motility & secretion
- Inhibit absorption in intestine
- Used to treat for osteoporosis as well (decrease resorption)
Activated Vitamin D3
- also known as 1,25-dihydroxycholecalciferol (1,25-DHCC)/calcitriol
- is formed in the skin as a result of UV rays
- increase sunlight, increase Vit D
Synthesis
- Cholecalciferol is converted to 25-hydroxycholecalciferol in the liver
- converted to 1,25-dihydrocholecalciferol in proximal tubule (requires PTH)
Calcium automatically converts 25 DHCC to 1,25 DHCC. At higher calcium concentrations, activated D3 (1,25-DHCC) is converted to 24,25 DHCC.
Actions of Vit D3
- Increase intestinal calcium absorption
- increase calcium binding protein in the intestine
- brush border
- rapid phase: via increased Na/Ca exchange activity
- slow phase: via increased synthesis of calcium binding protein (calbindins)
- Increase phosphate absorption
- Increase calcium & phosphate reabsoption in kidneys
- Increase calcium transporters thru cellular membranes in bone
- increases bone resorption
- In smaller quantities, Vit D promotes bone calcification
Other non-classical actions, read up Calcium homeostasis lecture notes.
_____________________________________________________________________
Hypoparathyroidism (Insufficient PTH)
- Decreased bone resorption & osteocytic activity
- Decrease calcium in ECF (hypocalcemia)
- Increased neuromuscular excitavility
- Na+ channel remain open, Na+ enters myocytes and cause increased excitability –>
- tetanic muscle contractions
- spasm of laryngeal muscle (laryngeal stridor)
- seizures (brain)
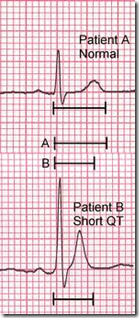
- Cardiac effect (repolarization is delayed with prolonged QT interval)
- *Cataract (protein accumulation)
- Dry & flaky skin
- Brittle nails
- tetany in the hand (Trousseau sign of latent tetany)
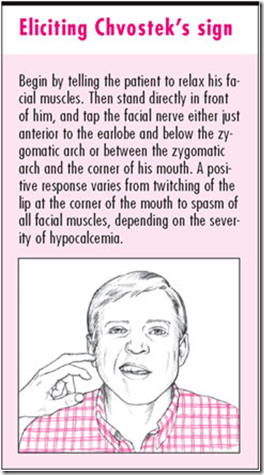
- Chvostek sign
Image: Trousseau sign of latent tetany
- carpopedal spasm
- sometimes hidden, seen suddenly when inflate BP cuff (decrease blood flow)
Image: Chvostek sign
Pseudo hypoparathyroidism
- Target organs (bone, kidney & intestine) receptors are resistant to PTH
- Congenital defect in the G protein
- associated with PTHR1
- Plasma Ca2+ low
- Plasma phosphate high
- Basic phosphatase activity is high
Primary hyperparathyroidism
- Excess PTH –> hypercalcemia, low phospahe
- Tumour, adnoma or hyperplasia
- Ectopic tumour in mediastinum
- More common in woman
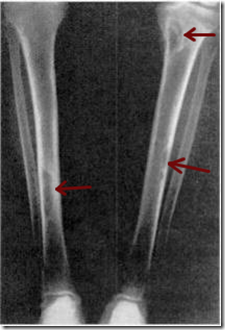
- Large cystic area in bone, may contain fibrous tissue
- Marrow fibrosis
- Bone disease: osteitis fibrosa cystica
- Metabolic acidosis (effect on renal tubule H+ reabsorption)
- Increased alkalline phosphatase (from osteoblasts, due to increased osteoblastic activity)
Image: Osteitis fibrosa cystica
Hypercalcemia with hyperparathyroidism (not very important)
MOANS, GROANS, BONES, STONES
- Psychic moans
- Depression of nervous system
- slow reflex
- depression
- Abdominal Groans
- Decreased appetite, anorexia, constipation, vomiting
- Bones
- Osteitis fibrosa/arthritis
- Parathyroid poisoning & metastatic calcification
- Calcium phosphate crystals throughout body
- Kidney stones (deposit in kidney)
- Shortened QT interval
Hypercalcemia can also be due to thiazide diuretics.
Secondary hyperparathyroidism
- As a compensation for hypocalcemia
- Increase in PTH –> hyperparathyroidism
Tertiery hyperparathyroidism
- After prolonged 2ndary hyperparathyroidism
- 2ndary hyperparathyroidism no longer responsive to treatment
- PTH related peptide (PTH-rp)
- binds to PTH receptor
- actions similar to PTH –> results in hypercalcemia
- PTH levels: low/undetected
- Produced by cancers
- Useful for: bone development, mammary gland development, lactation and tooth eruption






Vitamin D is really needed so that we can absorb properly the calcium and magnesium that we are taking from food and other supplements. ;”‘.,
Our very own online site
http://www.melatoninfaq.com/
Can someone please give me a refrence on the information on homeostasis of calcium in the blood, as i would love to use this information for my assignment but i cant unless i have the proper information on who wrote this information. Thanks