Coma
- Definition
- A state of prolonged unconsciousness characterized by loss of reaction to external stimuli or, a state of unrousable unresponsiveness.
- Differentiate from:
- Stupor
- Unconscious but can be aroused with repeated stimuli.
- Delirium
- Confused state often with restlessness and hallucinations.
- ‘Locked-in’ syndrome
- actually conscious but unable to speak or move
- may move eyes (massive brainstem damage)
- Vegetative state
- apparently awake but unresponsive (brainstem intact but widespread cortical damage)
- may breath spontaneously.
The Reticular Activating System
- Consciousness is determined by the reticular activating system
- which is located in the brainstem
- and its ascending connections
Coma is considered a medical emergency:
- Keep the patient alive
- resuscitate if necessary
- Exclude obvious factors
- head injuries
- hypogylcaemia, etc.
- Obtain history
- eyewitnesses
- medical information cards
- eg. MedicAlert
- Do general and neurological examination
- Do appropriate investigations
Causes of Coma
- Neurological
- Lesions within the brainstem
- affecting the reticular activating system
- Lesions in other parts of the brain
- compressing the brainstem
- Traumatic Brain Injury
- Diffuse brain injury
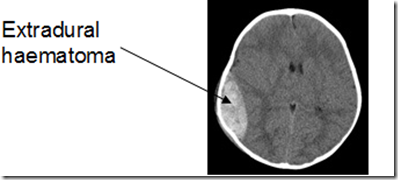
- Extradural (epidural) haemorrhage
- Haematoma – blood collection between the skull and the dura
- This is due to trauma resulting in rupture of arteries or veins
- commonly the middle meningeal artery
- Treatment is to evacuate the haematoma by drilling a burr hole.
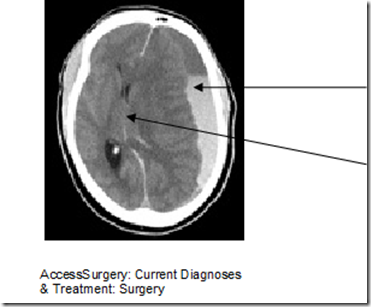
- Subdural haemorrhage
- The haematoma is between the arachnoid and the dura
- They are due to rupture of the bridging veins between the cerebral cortex and the venous sinuses
- Mid-line shift
- Ipsilateral ventricle effaced
- Acute or chronic
- chronic subdural haematomas become isodense (darker appearance)
- Vascular (eg. stroke)
- majority do not result in coma
- large strokes can act as mass lesions
- Infections (eg. encephalitis)
- Intracranial tumours
- Epilepsy/Post-Ictal states
- Hypertensive encephalopathy
- Toxic, metabolic, inflammatory or vascular conditions diffusely affecting the brain
- Hypoxia, CO2 Narcosis
- Drugs / Poisons
- Hypoglycaemia, Hyperglycaemia
- Hepatic Encephalopathy
- Electrolyte Abnormalities /Uraemia
- Endocrine: Myxoedema, Addisonian
- Liver Failure (portosystemic encephalopathy)
Types of coma
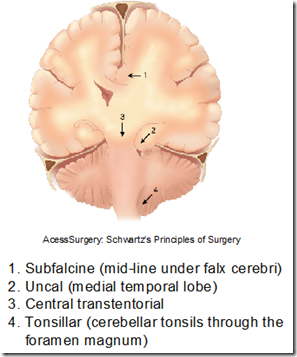
Coma due to mass lesions
- Hematoma, large strokes ( a type of mass lesion)
- compress brain tissue causing:
- herniation of brain tissue from one compartment to another
Hypoglycaemic coma
- Signs & Symptoms
- blood glucose < 3.0 mmol/L
- Sympathetic:
- sweating
- tremors
- palpitations
- anxiety
- Neuroglycopenia
- confusion
- abnormal behaviour
- coma
- death
- Causes
- oral hypoglycaemic agent/insulin in treatment of diabetes
- Give glucose immediately
- IV if patient drowsy or unconscious
- Whipple’s Triad
- Symptoms known or likely to be caused by hypoglycemia
- A low plasma glucose measured at the time of the symptoms
- Relief of symptoms when the glucose is raised to normal
Hyperglycaemic comas
- There are two types of hyperglycaemic comas in diabetes:
- Diabetic Ketoacidosis (DKA)
- Type 1 diabetes
- Hyperosmolar Hypergylcaemic Non-Ketotic Coma (HHNC)
- Type 2 diabetes
- The new term is: HHS or Hyperosmolar Hyperglycaemic State. However only about 20% of HHS have coma
Drugs & Coma
- Drug overdose may be accidental or intentional
- Diagnosis
- History important
- Suspect if
- IV needle marks
- pin-point pupils
Liver Failure (Portosystemic Encephalopathy)
- In liver failure
- there is accumulation of ammonia in the systemic circulation
- leading to coma
- It may occur in
- Acute liver failure
- acute fulminant hepatitis
- paracetamol overdose
- Chronic liver disease
- alcoholics
- chronic hepatitis B, C
- Specific signs to look for
- Early
- Drowsiness
- confusion
- altered sleep pattern
- fetor hepaticus
- Asterixis
- flapping tremor
- constructional apraxia
- loss of the ability to execute or carry out learned purposeful movements
- despite having the desire and the physical ability to perform the movements
- disorder of motor planning
- Late
- Coma
- +ve Babinski signs
CNS infection & Coma
- Serious Infections
- Encephalitis
- Meningitis
- Brain abscess
- Suspect if
- fever
- headache
- progressive drowsiness
- fits prior to coma
- Physical signs of neck stiffness
- meningism in meningitis
- Papilloedema
- may be present indicating raised intracranial pressure
_____________________________________________________________________
Postures found in comatose status
*Refer posture and balance lecture
Decerebrate Posture
- Brainstem Injury
- Extension of arms with internal rotation
- Pronation of wrists and flexion of fingers
- Legs extended with plantar flexion of feet
Decorticate Posture
- Lesions above brainstem
- Arms adducted and flexed across the chest
- Wrist and fingers flexed
- Legs extended with plantar flexion of feet
_____________________________________________________________________
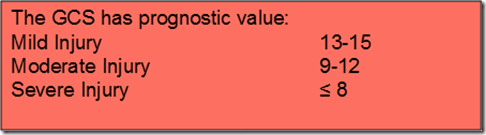
Glasgow Coma Scale
Measure consciousness
- Based on 3 clinical responses: (EVM)
- Eye Opening
- Verbal Response
- Motor Response
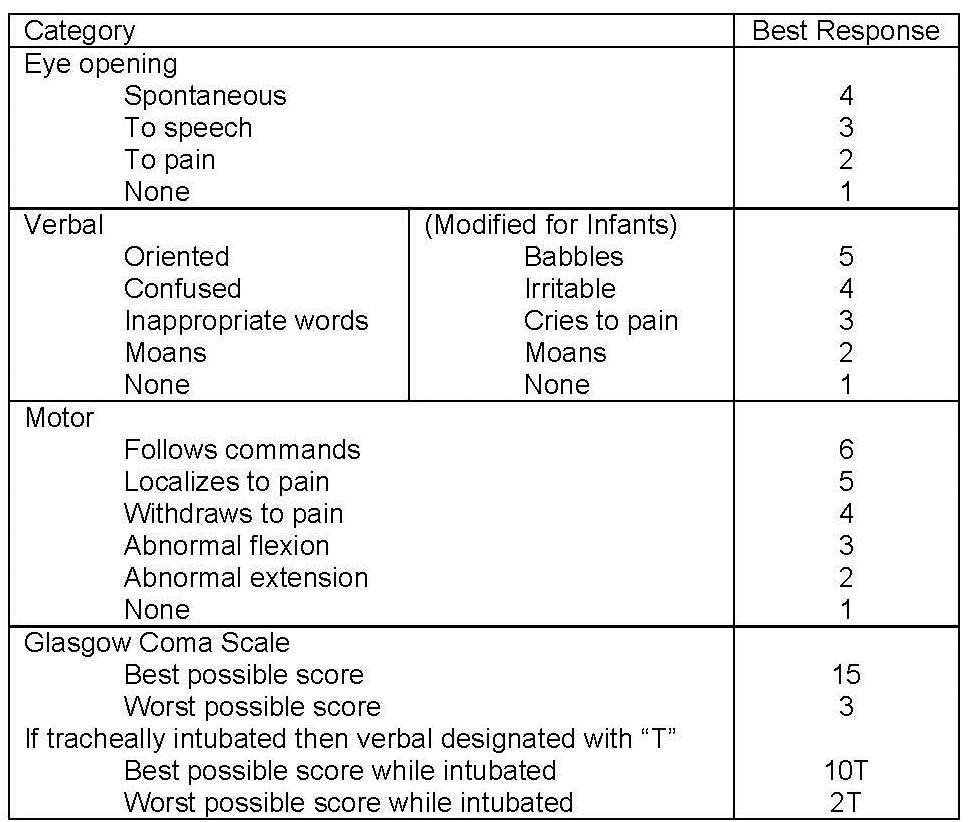
- Record the best response
- Minimum Score 3
- Maximum Score 15
- Chart initial and subsequent scores
- The GCS record is the patient’s change in conscious level with time.
_____________________________________________________________________
Brain death
- Definition
- A condition in which there is:
- Permanent and irreversible loss of the functions of the brain
- together with irreversible loss of the capacity to breathe
- This person is supported by:
- Artificial mechanical ventilation
- Other supportive measures
- A person certified to be brain dead is considered to be legally dead
- Criteria
- Coma
- No spontaneous respiration
- No response to external stimulation
- Absence of brainstem reflexes
- Ethical issues
- Medicolegal
- who has the right to determine who should be kept alive by life support?
- Beneficence
- the duty of the doctor to do good
- Justice
- How is it justified?
- How is healthcare distributed under circumstances of limited human and financial resources and who / how determines
- ‘who gets what’?
- Dignity
- Everyone has a right to a dignified death
- Autonomy
- What would the patient have wanted?
- Many countries now have legal and medical definitions for brain death:
- The patient is in apnoeic coma on a ventilator
- There is evidence of a significant medical or CNS event that would result in brain death
- Formal tests of brainstem function confirm absent brainstem reflexes
- Before diagnosing brainstem death exclude:
- Hypothermia (T<35°C)
- Drug Intoxication
- Acid-Base Imbalance
- Electrolyte Abnormality
- Hypoglycaemia/Endocrine Disorder
- Tests of brainstem death:
- No pupillary response to light
- pupils fixed
- No oculocephalic reflex
- Doll’s Eye
- No vestibulo-ocular reflex
- No motor response within cranial nerve distribution
- No corneal reflex/gag reflex/grimacing to painful stimulus
- No cough response to pharyngeal/laryngeal/tracheal stimulation
- Apnoea with no respiratory effort when ventilator is switched off & PaCo2 rises to above 6.7kPa (50mmHg)
- Tests of brainstem death must be done twice at least 6-24 hours apart
- Tests must be done independently by 2 different senior doctors, one of whom must not be in the medical team managing the patient
- EEG is not routinely required
- Once the diagnosis is established, inform the next-of-kin and explain the diagnosis
- Allow adequate time for the family to understand and discuss the issue amongst themselves
- Informed consent must be obtained before withdrawing life support
- In suitable cases discuss and obtain informed consent from next-of-kin for organ donation
- Members of the surgical transplant team and the medical team looking after the potential recipient should not be involved in certification of brain death of the donor and in counselling / obtaining consent from the donor’s next-of-kin regarding organ transplantation


Thank you for this, I found it really useful!