Peripheral nerve injuries
- Due to
- Trauma
- acute compression
- Signs & symptoms
- Loss of motor function
- Loss of sensory function
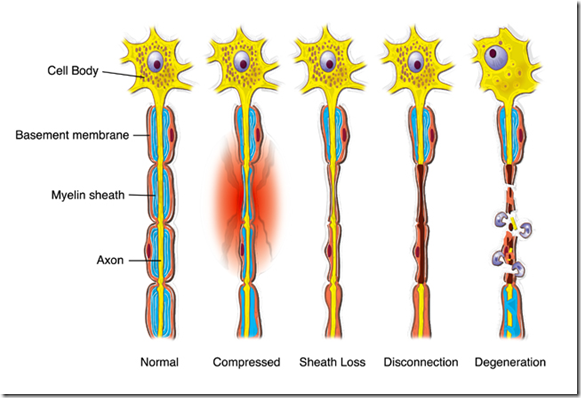
- Pathology
- Demyelination/axonal degeneration
- Disruption of the sensory/motor function of the injured nerve
- Remyelination with axonal regeneration
- Reinnervation of the sensory receptors & muscle end plates
Degenerative changes
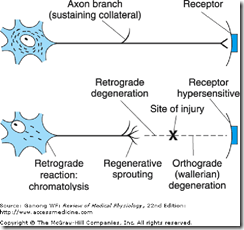
- Axonal injury
- Degenerative changes at proximal & distal end
- Anterograde degeneration (Wallerian Degeneration)
- Affecting the
- Injured neuron
- Neurons functionally connected to the injured neuron
- Transneural degeneration
- also degenerate neurons that synapses with the injured neuron
- Starts in 24 hours
- Affecting the
- Retrograde Degeneration
- Extends up to the first node of Ranvier proximal to the injury
- Changes in the dendritic tree
- the parent cell body & the part of the axon still attached to the cell body
- Chromatolytic changes
- Swelling of the cell
- Displacement of the nucleus to periphery
- sometimes extruded out
- Fragmentation & reduction of Golgi apparatus
- Disappearance of neurofibrils
- Anterograde degeneration (Wallerian Degeneration)
- Degenerative changes at proximal & distal end
Chromatolysis
- disintegration of the Nissl substance
- begins within 24 – 48 hours
- begins near the axon hillock & spreads to other parts
- occurs in certain infectious or degenerative diseases of the nervous system
- poliomyelitis
- progressive muscular atrophy
- degree of chromatolysis depends on
- proximity of the site of injury to the nerve cell
- more in motor neurons
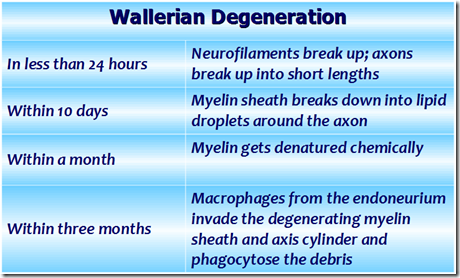
Wallerian degeneration
Process that results when a nerve fibre is cut or crushed, in which the part of the axon separated from the neuron’s cell body degenerates.
Pre-degeneration reactions – 1st things that happen when there is injury
- Decentralisation of the nucleus
- increased ribosomes surrounding the nucleus
- Immune response
- Macrophages start attacking the Schwann cells of the distal segment
- Nervous system reaction
- All adjacent neurons start extending sprouts of their axons
- towards the injured neuron
- Enzymatic Action
- The axon of the distal segment is broken down by enzymes
Pathophysiology
- Axonal degeneration
- Axis cylinder (axolemma) swells & breaks up into small pieces
- Enzymatic Action
- The axon of the distal segment is broken down by enzymes
- the products of this action is carried by retrograde transport to the soma
- The axon of the distal segment is broken down by enzymes
- Debris appear in the space occupied by axis cylinder
- Enzymatic Action
- Myelin sheath disintegrate into fat droplets
- Neurilemmal sheath intact
- Axis cylinder (axolemma) swells & breaks up into small pieces
- Myelin clearance
- Immune response
- Macrophages start attacking the Schwann cells of the distal segment
- Macrophages invade & remove the debris of axis cylinder
- Immune response
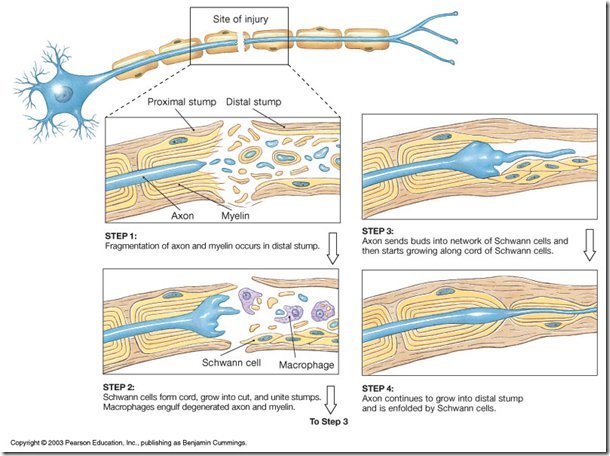
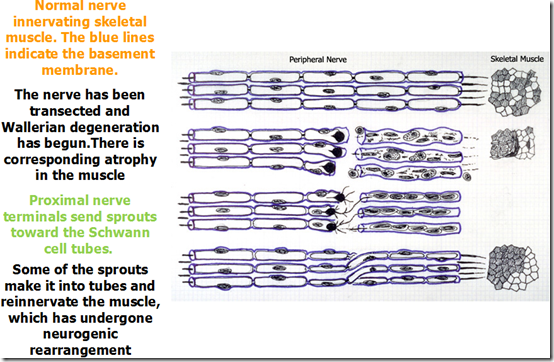
- Regeneration ( begins about 20 days after injury)
- Schwann cells multiply
- Macrophages produce interleukin-1 which stimulates Schwann cells to secrete substances that promote nerve growth
- forms a solid cord of elongated cells within the endoneural tube –> towards the target tissue
- those that did not reach the target tissue will start dying
- growth path for axon
- Adjacent basal lamina separate
- creating an annular compartment
- Neurilemmal tube becomes empty
- now filled by cytoplasm of Schwann cells
- Axonal sprouts (neurofibrils)
- Neurofibrils grow out in all directions from the proximal axon
- Sprouts grows into the distal annular compartment
- All but one axonal sprout degenerate
- Surviving fibril enlarges to fill the distal tube Regenerated fiber rarely attains a fiber diameter more than 80% of normal
- Schwann cell form myelin sheath around the reinnervating axonal sprout
- Sheath begins to develop in about 15 days
- Myelin sheath is completed in one year
- Regeneration in the cell body
- Nissl granules reappear
- Golgi apparatus reappear
- The cell regains its normal size
- Nucleus returns to central position
- Schwann cells multiply
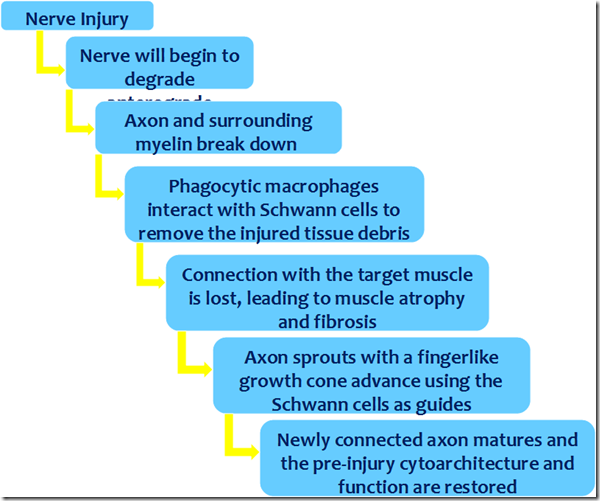
Summary:
Transneural degeneration
- This neuron is not the one that is injured
- Optic nerve injury leads to degeneration of the lateral geniculate body
- Injury to posterior nerve root leading to degeneration of dorsal horn of spinal cord
Changes in nerve degeneration
- There will be neurogeneic rearrangement
- the growing axon does not necessarily follow the expected growth path
- incomplete nerve regeneration
- Criteria for complete nerve regeneration
- Gap between cut ends of neuron
- should not be greater than 3mm
- Neurilemma should be present
- Nucleus must be intact
- should not be extruded
- Two cut ends should remain in the same line
- or else there will be rearrangement
- Nerve regeneration is generally limited
- because axons become entangled in the area of tissue damage
- Neurotropins
- nerve growth factors – influence nerve regeneration
- Growth factors produced by neurons, glial cells, Schwann cells, and target cells
- Gap between cut ends of neuron
_____________________________________________________________________
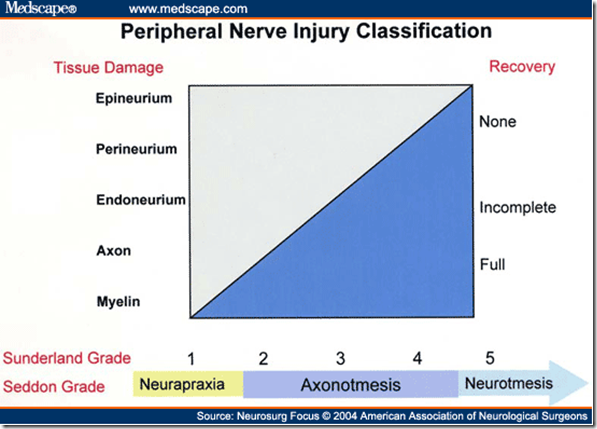
Classification of nerve injuries
Seddon’s classification (3 types)
- Neuropraxia
- Caused by
- minor nerve stretch/pressure
- causing ischemic injury to the nerve
- Results in conduction block
- without any structural damage
- minor nerve stretch/pressure
- Electrodiagnostic study
- normal – above and below the level of injury
- No denervation muscle changes are present
- Recovery
- Once remyelinated, complete recovery occurs
- Caused by
- Axonotemesis
- Caused by
- excessive stress injury to the nerve
- Pathology
- The basal lamina of Schwann cells & other sheaths are intact
- The epineurium & other supporting structures are not disrupted
- internal architecture is relatively well preserved
- Cause Wallerian degeneration distal to the injury
- Endoneural tubes remain intact
- Electrodiagnostic studies
- denervation changes in the affected muscles
- Recovery
- In cases of reinnervation
- motor unit potentials (MUPs) are present
- Once remyelinated
- complete recovery with axons reinnervating their original motor and sensory targets
- In cases of reinnervation
- Caused by
- Neurotemesis
- Caused by
- penetrating injury to the nerve
- Pathology
- All the sheaths are disrupted
- Physical gaps in the nerve may occur even though an epineurial sheath appears in continuity – after traction or crush
- Recovery
- No recovery unless repair is undertaken
- Unrepaired nerve will be completely replaced by fibrous tissue
- there is complete loss of anatomic continuity
- Caused by
Sunderland’s classification (6 degrees of nerve injury)
| 1st degree (neuropraxia) |
|
| 2nd degree (axonotemesis) |
|
| 3rd degree |
|
| 4th degree |
|
| 5th degree |
|
| 6th degree |
|
Tinel sign
- Light percussion on the nerve with a patellar hammer
- from distal to the proximal end
- A tingling sensation is experienced at the level of regeneration
- As the regeneration of the axon grows, the level of tingling sensation also shifts
- Absent in neuropraxia
Denervation hypersensitivit
y
- Following a section (cut) of a motor nerve
- Pathology
- A deficiency of chemical messenger (due to denervation) generally produces an up-regulation of its receptors
- Acetyl choline receptors increase
- more than 10 folds in number
- dispersed over the entire surface of the sarcolemma
- Sensitivity of the receptors towards acetylcholine increases
- (desperate to be innervated)
- Denervation also lowers the membrane potential
- Muscles more prone to fibrillations
- After regeneration
- functional innervation of the muscle is reestablished and sensitivity to acetyl choline decreases
- resting membrane potential is restored
- fibrillation disappears after regeneration
- Other muscles
- Smooth muscle
- does not atrophy when denervated
- becomes hyperresponsive to the chemical mediator that normally activates it
- Denervated exocrine glands [except sweat glands]
- become hypersensitive
- due to the synthesis or activation of more receptors
- A deficiency of chemical messenger generally produces an up-regulation of its receptors
- Lack of reuptake of secreted neurotransmitters because pre-synaptic nerve is not present
- Therefore excess neurotransmitters in the ‘synaptic space’ –> hyperreactivity of muscles
- Multiple sclerosis
- Demyelination of oligodendrocytes in the central nervous system & Schwann cells in the peripheral nervous system
- Disruption of connection between upper motor neurons & the lower motor neurons
- Can cause
- increased muscle tone
- difficulty controlling muscles
- exaggerated reflexes
- muscle spasms
- Smooth muscle


its very hard
That is so helpful!
thanks
thnx it’s realy thankful
??