
- Definition
- A chronic bacterial disease of the skin, peripheral nerves and the upper airway
- One of the most feared diseases
- Causal organism
- M. Leprae
- Early stage
- painless depigmented patch
Differential diagnosis
- Tinea vesicolor
- Pityriasis rosea
- Birth mark depigmentation
- Granuloma multiforme
- Psoriasis
- Contact dermatitis
- Avitaminosis B
- Neurofibromatosis
- Scleroderma
- Xathomatosis
Epidemiology
- Infectious agent:
- Mycobacterium leprae
- acid fast bacilli
- cannot grow in bacterial media/culture
- Grow on
- mouse foot pads
- in nine banded armadillo
- Mycobacterium leprae
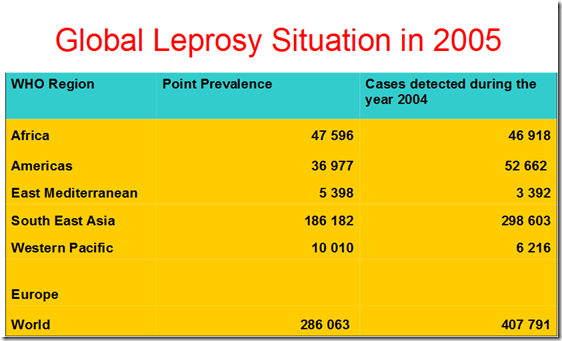
- Occurrence
- World prevalence 10-12 million
- Prevalence rates >5 per/1000 rural tropics and subtropics
- Endemic areas
- SE Asia
- South Asia
- Philippines
- Indonesia
- India
- Bangladesh
- Pacific Islands
- Tropical Africa
- Latin America
- Reservoir
- Man is the only reservoir of proven significance
- Feral Armadillos in Louisiana & Texas are affected
- Naturally acquired leprosy Manageby monkey & chimpanzee
- captured in Nigeria and Sierra Leone\
Mycobacterium leprae
- General
- Acid fast
- occurs in intracellular and extracellular
- Occurs in clumps or bundles
- globi
- Affinity for
- Schwann cells
- cells of the reticulo- endothelial system
- They remain dormant in various sites
- can cause relapse
- Leprosy is highly infectious disease
- but low pathogenecity
- Acid fast
- Mode of transmission
- Contact
- not clearly established
- Household
- prolonged close contact
- not clearly established
- Droplet infection
- Millions of bacilli are liberated daily
- in the nasal discharge
- remain viable for 7days in dried nasal secretions
- Cutaneous ulcers also shed large amounts of bacilli
- in the nasal discharge
- Millions of bacilli are liberated daily
- Contact
- Incubation Period
- 9 months – 20 years
- average 4 years for tuberculoid
- 3-5 years for lepromatous
- Disease seen children <3 years
- 50 cases so far
- youngest: 2 1/2 month
- 9 months – 20 years
- Period of communicability
- Infectivity is lost in most instances (continuous & regular treatment)
- within 3 months
- with Dapsone (DDS) or clofazimine
- within three days
- with rifampine
- within 3 months
- Infectivity is lost in most instances (continuous & regular treatment)
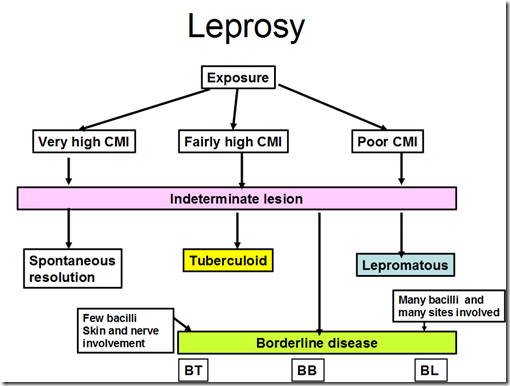
- Susceptibility and resistance
- Persistence and form of leprosy depend upon ability to develop cell mediated immunity
- Lepromin test
- Intradermal injection of autoclaved M. Leprae & the presence or absence of induration at 28 days is called Mitsuda reaction
- Reaction
- lepromatous leprosy
- -ve immune reaction
- Mitsuda reaction
- tuberculoid disease
- +ve immune reaction
- lepromatous leprosy
- The test gives prognostic information but it is not diagnostic
Intermediate lesion
- Small macules
- irregular
- raised edge
- pale skin lesions
- anywhere on the body
- Most common on
- back
- forearm
- thighs
- face
- Most common on
- No sensory loss
- Normal sweating
- Pathology –non specific inflammatory reaction
- 90% spontaneous recovery
- may progress to any of the three later types
- depending on the cell-mediated response
- Tuberculoid leprosy
- Lepromatous leprosy
- Borderline leprosy
_____________________________________________________________________
Tuberculoid leprosy
- Clinical features
- One or more sensationless asymmetrical macules with raised edges
- In dark skins macules: depigmented
- in pale skins macules: reddish
- Affected nerves are thickened
- ulnar
- median
- superficial radial
- Loss of sweat
- Loss of sensation
- Wasting of muscles
- One or more sensationless asymmetrical macules with raised edges
- Skin smear
- -ve for M. leprae
- Biopsy shows
- epithelial granuloma with giant lymphocytes
- scanty bacilli
Lepromatous leprosy
- Clinical features
- Numerous symmetrical distributed, macular, plaque form/nodular skin lesions
- Leonine facies
- lion face
- Skin thickened by infiltration
- Swelling of nose, ear and lips
- Leonine facies
- Proliferation of infection in mucous membranes
- causes nasal congestion & keratitis
- Nasal discharge, painful eyes
- Peripheral neuritis
- complicated by neuropathies ulcers on limbs
- lead to disfiguration and disability
- Loss of sensation, pain and temperature
- Neuropathic ulcers on
- hands, feet
- with loss of fingers and toes
- Painless burns or ulcers
- Secondary infection
- Facial nerve palsy
- Testis & lymph nodes may be damaged
- Generalized systemic symptoms
- fever
- Numerous symmetrical distributed, macular, plaque form/nodular skin lesions
- Skin smear highly +ve for bacilli
- Immune response highly -ve (Mitsuda reaction)
Borderline leprosy
- between tuberculoid & lepromatous
- Mixed clinical features
- Skin lesions often raised ring shaped lesions
- with normal or slightly reduced sensation
- Peripheral nerves may be thickened
- Skin lesions often raised ring shaped lesions
_____________________________________________________________________
Clinical manifestations
- Signs of peripheral nerves involvement
- Skin lesions
- Test for light touch, pin prick & temperature discrimination
- Hyperesthesia & anesthesia
- Peripheral nerves
- Bilateral palpation of peripheral nerves for enlargement and tenderness
- ulnar at elbow
- peroneal nerve at head of fibula
- great auricular nerve
- Bilateral palpation of peripheral nerves for enlargement and tenderness
- Muscles
- Paralysis
- muscle wasting
- Trophic ulcers
- Skin lesions
Diagnosis
- Clinical examination
- Examination of
- skin
- nerves
- pain sensation
- sweating
- motor functions
- nerve thickening
- Examination of
- Laboratory Examination
- Skin slit smears
- Skin is slit without drawing blood
- smear taken & stained for bacilli
- usually from ear lobes
- The quantity and the morphology is measured
- Skin biopsy
- of lesion edge/nerve
- Mitsuda reaction (Not diagnostic)
- Skin test with lepromin
- made from autocalved Mycobacterium leprae
- Granulomatous nodule after 28 days in tuberculoid and some boderline cases
- Healthy persons may show a positive Mitsuda reaction
- If no reaction –> lepromatous leprosy
- Skin test with lepromin
- Skin slit smears
Treatment
Multidrug therapy (MDT)
- Combinations of
- Rifampicin
- urine slightly reddish for few hours
- Clofazimine
- brownish black discoloration
- drness of skin
- Dapsone
- allergic reaction towards sulpha drugs
- itchy skin rashes
- exfoliative dermatitis
- do not give to patients who are allergic
- allergic reaction towards sulpha drugs
- Rifampicin
- May develop drug resistance if only 1 drug used
_____________________________________________________________________
Reactions in leprosy
Non-Lepromatous lepra reaction (Type 1 lepra reaction)
- Seen following treatment of boderline leprosy
- Type 4 delayed hypersensitivity reaction
- Last for few days to several weeks
- Reactions
- Acute inflammation of preexisting borderline lesion
- Skin lesions become swollen and erythematous
- Neurological lesions
- ulnar nerve palsy may occur abruptly
- Both upgrading or reversabile reaction
- more tuberculoid or more lepromatous
Erythema Nodosum Leprosum (Type 2 lepra reaction)
- Humeral antibody response to antigen antibody complex
- type III hypersensitivity reaction
- systemic manifestations
- Fever
- Athralgia
- Painful subcutaneous erythematous nodules
- Iritis
_____________________________________________________________________
Prevention & control of leprosy
- Primary prevention
- Health promotion
- improve housing standards
- standard of living
- BCG (Limited protection)
- Secondary prevention
- Early diagnosis & treatment
- WHO-Multi drug treatment
- follow up 5 years,
- Tuberculoid – 6 months
- Borderline & lepromatous – 2 years
- Tertiary prevention
- Disability limitation
- Care of the hands, feet, neuropathy and loss of sight
- Rehabilitation
- Restoration of function
- Deformities, loss of limbs fingers, nose etc
_____________________________________________________________________
Poliomyelitis
- Definition
- An acute viral infection
- with severity ranging from inapparent infection to non-specific febrile illness, aseptic meningitis, paralytic disease and death
- Minor illness includes (if the disease progresses)
- fever
- malaise
- headache
- nausea
- vomiting
- Severe illness includes
- muscle pain
- stiffness of neck
- stiffness back with/without paralysis
- The site of paralysis depends upon the location of the nerve cell destruction in the spinal cord/the brain stem
- An acute viral infection
- Infectious agent
- Polio virus Type 1
- Brunhilde
- most commonly seen in epidemics
- Type 2
- Leon
- Type 3
- Lansing (genus Enterovirus)
- Polio virus Type 1
Epidemiology
- Occurrence
- Worldwide
- disease of children & adolescents
- Reservoir
- Man only
- people with inapparent infections
- Man only
- Mode of transmission
- Direct contact through close association
- Rare instances – fecaloral route
- Incubation period
- 7-14 days of paralytic cases
- Range 3-35 days
Susceptibility and resistance
- Susceptibility to infection is general
- paralytic infections are rare
- immunisation at birth
- Infants born to immune mothers have transient passive immunity Injections of other vaccines may provoke paralysis
- Second attacks are rare
- due to different type of polio virus
- during the prodromal phase
- 90% have no or almost no symptoms/indistinguishable from influenza
- 9% have non-paralytic polio
- 1% have spinal/bulbar polio
- 10% die
- 50% recover fully
- 40% are left with only partial recovery/permanent paralysis
- 0.4% of permanent paralysis,
- 1 or both lower limbs
- 0.01%
- Quadriplegia
- respiratory paralysis
Pathophysiology of polio
- Polio is generalized infection
- which may involve the whole body including muscles, liver spleen, and gastrointestinal system
- Anterior horn cells are chiefly affected
- Degeneration & loss of Nissls granules
- uptil complete disappearance of the cells
- This results in the lower motor neuron paralysis
- with asymmetrical paralysis & normal sensation
- Paralysis occurs in small proportion & may be minimal to severe
- Paralysis may cause shortening & decrease diameter of the bones
- Most common muscles involved
- extensor of hips
- extensor of knees
- dorsiflesion of ankles
- deltoid
- triceps
- thenar muscles
- respiratory muscles
- spinal muscles
- Degeneration & loss of Nissls granules
- Bulbar paralysis
- Pharyngeal paralysis
- inability to swallow food, drinks and own secretions
- inability to cough and difficulty in speaking
- Pharyngeal paralysis
- Respiratory paralysis
- Respiratory muscles rare
- Intercostal muscles
- Anterior horn cells of the thoracic region
- Diaphragm
- Anterior horn cells of mid cervical
- Fibrillations of muscles
- Paralyzed muscles show fine ripples of contractions
Diagnosis of polio
- Clinical examination
- confirmation of sudden onset of acute flaccid paralysis (AFP)
- with no loss of sensation
- confirmation of sudden onset of acute flaccid paralysis (AFP)
- Laboratory culture (stool)
- isolate virus
- 100% isolation of virus within 2 weeks of onset
- WHO criteria for certification of polio free
- 50% within three weeks of onset
- 25% within 6 weeks
- 100% isolation of virus within 2 weeks of onset
- isolate virus
Prevention of polio
- Primary prevention
- Health education
- Oral polio virus vaccine (OPV)
- Live attenuated Sabin Vaccine
- OPV given in Malaysia in
- 2nd month
- 3rd month
- 5th month
- Booster
- 18 months
- standard 1
- Intramuscular injection
- Salk Vaccine
- Secondary Prevention
- Early diagnosis and prevention
- Spinal polio and bulbar polio
- Disability limitation
- avoid factors that potentiate paralysis
- eg. operations, injections & strenuous exercise
- Prevention of deformities & contractures (of bone?)
- Early diagnosis and prevention
- Tertiary prevention (Rehabilitation)
- Surgery on contractures
- equinus foot
- wheel chair for the disabled
Eradication of polio
- Polio transmission is now limited to about 9 countries
- Afghanistan
- Pakistan
- India
- Angola
- Congo
- Nigeria
- Somalia
- Ethiopia
- Sudan
- Eradication is possible because the virus affects only humans
- no animal reservoir
- no long term carriers
- virus cannot survive outside the human body for long
- Acute flaccid paralysis (AFP) is being carried out all countries that have declared free of polio
- Malaysia is free of polio





Thanks
That one of the best paper on leprosy. As, I am medical student at Westminster university. I am suppose to do a poster on leprae due next week, can I have permission to use one your diagram in my presentation?
antoine
Sure! Please feel free to use any of the materials in this medical blog!
This was very a very informative post. Thank you!