Definitions:
- Seizures
- occasional, sudden, rapid and local discharges of gray matter
- Epilepsy
- brain disorder characterised by periodic, unpredictable occurrence of seizures
Seizures
- Transient changes of behaviour
- due to disordered, synchronous and rhythmic firing at high frequency of groups of neurons from the cerebral cortex
- When seizure activity is initiated at local focus (cortex, hippocampus, thalamus)
- invades normal brain tissue to involve both parts of the cerebral hemispheres
- a generalised convulsion/seizure occur
- Can be preceded by an aura
- tingling
- numbness of limbs
- hallucinations
- followed by convulsions
- involuntary skeletal muscle movements
- loss of consciousness
- After an attack
- post-ictal depression
- patient is confused, drowsy and has headache
- post-ictal depression
- Abnormal electrical activity during and after a seizure can be recorded using electrodes placed on the scalp. Called the electroencephalogram (EEG)
- it shows characterisitic features for various types of seizures
- Repeated epileptic attacks can cause neuronal death
The symptoms of an epilepsy attack depends on
- the site of the primary abnormal electrical discharges
- the extent of their spread
Range of epilepsy attack severity
- A seizure attack may range from a brief lapse of attention to a full convulsive fit with jerky movements.
- The patient may become unconscious for a short time, have a change in perception and experience odd sensations or behaviours
- Others may exhibit repetitive movements like blinking or twitching
When abnormal activities (seizures) involve the:
- motor cortex
- convulsions occur
- hypothalamus
- peripheral autonomic effects occur
- reticular formation of the upper brain stem
- consciousness is lost
Classification of seizure types
Generalised seizures
Seizure activity affect both brain hemispheres
- Generalized tonic-clonic (grand mal) seizures
- loss of consciousness
- tonic muscle contractions
- alternating with clonic contractions (lasting 1-2 minutes)
- Absence (petit mal) seizures
- abrupt onset of impaired consciousness
- with staring
- cessation of ongoing activity
- lasting less than 3 seconds
- resumption of activity on end of seizure
- with no awareness of seizure episode
- 3 Hz spike EEG. related to:
- Voltage regulated Ca 2+ current / low threshold
current (T-current)
- Voltage regulated Ca 2+ current / low threshold
- abrupt onset of impaired consciousness
- Tonic seizures
- Atonic seizures
- Clonic seizures
- Myoclonic seizures
- short ( 1 sec) shock-like contraction of muscle
- may be limited to 1 extremity/generalised
Partial (focal) seizures
seizure activity begins at a focal site in the cortex
- Simple partial seizures
- Manifestations depend on the region of cortex activated by the seizure:
- Motor cortex
- clonic jerking of left thumb
- Sensory (somatosensory) cortex
- paresthesia of left thumb
- Motor cortex
- Consciousness retained
- Manifestations depend on the region of cortex activated by the seizure:
- Complex partial seizures
- Loss of consciousness lasting 30sec – 2 min
- Associated with purposeless movements
- like lip smacking or hand wringing
- Partial seizures secondarily generalised (tonic-clonic)
- seizure affecting both brain hemispheres
- loss of consciousness
- tonic muscle contractions
- alternating with clonic contractions
- lasting 1-2 minutes
- Psychomotor epilepsy
- Focus on temporal lobe
- Stereotype
- purposive movement
- rubbing/patting movement
- behaviour
- dressing, walking, combing hair
- purposive movement
- Could have strong emotional response
- Seizure lasts few minutes
- no awareness of event on recovery
- Jacksonian Epilepsy
- focus of abnormal activity in the motor cortex
- Repetitive jerking of particular muscle group
- beginning on 1 side of body
- Thumb / big toe / angle of the mouth spreading to
involve other parts of the body within 2 min before
dying out
- Voluntary control of the affected parts are lost, but consciousness could be retained
Other types of seizures
- Infantile spasms
- Febrile seizures
- Status epilepticus
- continous seizure episodes
- life threatening
Implication of knowing types of seizure
- Importance
- predicting prognosis
- selecting treatment
- likelihood of finding underlying cause of seizure
- 3 stages to a seizure
- initiation
- synchronization of surrounding
- propagation
- recruitment of normal neurons
Cause of epilepsy
- no recognisable cause
- Develop from brain damage
- trauma
- infection
- tumour growth
- neurological diseases
Seizure provoking factors
- Missed medication
- Sleep deprivation
- Stress
- Alcohol & Drug abuse
- Over the counter medication
- Nutritional deficiencies:
- Vitamins and minerals
- The menstrual cycle
- Cycles of the moon
- Bright / flickering light
- Certain sound
Diagnosis of seizures
- Patient history
- Physical examination
- EEG
- Read from OLIS
- Imaging to localise seizure focus
- CT scan
- PET
- MRI
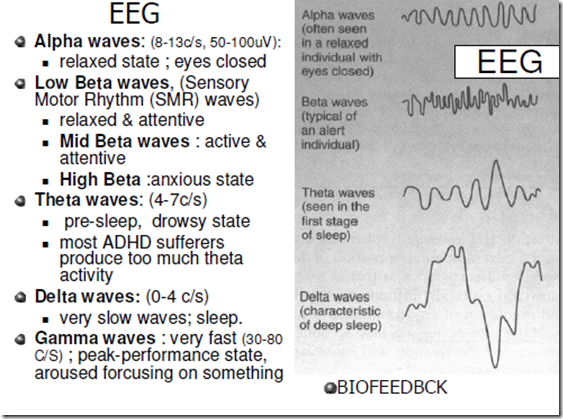
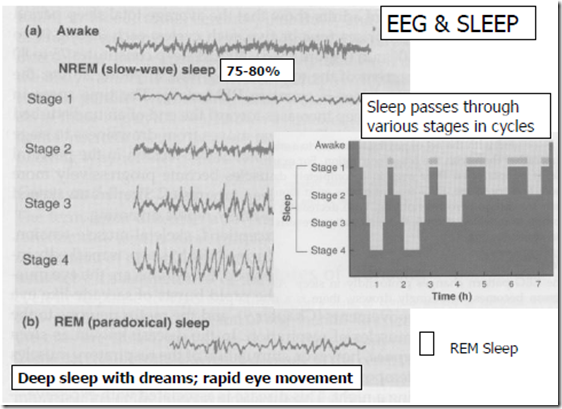
EEG
- Electroencephalography (EEG) is a test by which the electrical activity generated by the brain is recorded through thin wires placed on the scalp.
- Normal brain rhythms and any abnormal epileptic activity are reviewed on a computer screen or on paper.
- The EEG recording assists in determination of the seizure
type and epilepsy syndrome.
- In special circumstances, EEG may assist monitoring of treatment and help localise the seizure focus.
- EEG should be recorded and interpreted in a centre experienced in management of epilepsies and EEG
Main roles of EEG
- Help distinguish focal from generalised seizures and epilepsies
- Help localise the site of seizure activity in a child with focal epilepsy
- Help make a specific (syndrome) diagnosis
- Help confirm or exclude epilepsy, following a thorough clinical evaluation
- Monitor treatment in some types of epilepsy
Brain imaging
- Structural imaging (CT, MRI)
- exclude an underlying brain abnormality
- scar
- malformation
- tumour
- infection
- exclude an underlying brain abnormality
- Functional imagine (SPECT, PET, fMRI)
- assist localisation of a seizure focus and its relationship to important brain region
- usually in children considered for brain surgery
Epilepsy – Impact on patients
- The young
- interruption in their studies, activities, family, career
- Female patients
- antiseizure drugs on fetal development
- birth defects (spina bifida, cleft lip etc)
- antiseizure drugs cause liver enzyme induction
- failure of oral contraceptives
- increase risk of bone disease
- seizures may disrupt functions of estrogen
- decrease birth rate
- weight gain
- abnormal menstrual cycle
- cyst in ovaries
- antiseizure drugs on fetal development
Neurochemical basis of seizures
- Seizures associated with
- (-) inhibitory synaptic function (GABA)
- (+)excitatory synaptic function (Glutamate)
- Abnormal electrical properties of affected neurons
- seizures in experimental animals caused by:
- GABAa- antagonists (bicuculline, picrotoxin)
- Agonists of glutamate receptor subtypes (NMDA, AMPA,
kainic acid)
- seizures in expt animals alleviated (relieved) by:
- GABAa- agonists
- Antagonists of glutamate receptor subtypes (NMDA, AMPA, kinic acid)
- Post-mortem human brains:
- (-) glutamate in cells of focus
- (+) in cells surrounding focus
Antiseizure drugs
- Prolong sodium channel inactivation
- phenytoin
- carbamazepine
- lamotrigine
- phenobarbitone
- sodium valproate
- topiramate
- [-] rapid repetitive firing in isolated neurons
- Reduction of low threshold T-type Ca++ current which govern oscillatory responses in thalamic neurons
- ethosuximide
- Enhance GABAA activity to inhibit synaptic transmission:
- Direct action on GABA receptor-chloride
channel complex- benzodiazepines
- barbiturates
- topiramate
- Block reuptake or metabolism of GABA
- sod valproate
- gabapentine
- tiagabine
- vigabatrin
- Direct action on GABA receptor-chloride
- Reduce Glutamate transmission:
- Block of AMPA receptors
- phenobarbitone
- topiramate
- Block of AMPA receptors


good note i feel comfort by reading this note