Insulin
Biosynthesis & Structure
- 51 amino acids
- 2 poplypeptide chain linked by 2 disulphide linkages
- A
- B
- Human insulin gene on chromosome 11
2 preproinsulin –> proinsulin –> insulin + C peptide
Regulation of insulin secretion
Stimulation
- Increase in blood glucose
- Increase in amino acids
- Gastrointestinal hormones
- GIP
- CCK
- gastrin
- Pharmacological agents
- sulfonylurea
Inhibition
- hormonal factors
- alpha adrenergic agoinst
- epinephrine
Secretion of insulin (from stimulation of glucose)
- Increase in blood glocose
- glucose transported into beta cells
- by facilitated diffusion
- thru GLUT-2
- increase in glucose concentration in beta cells
- increase in glucose metabolism in beta cells
- increase in ATP:ADP ratio within the cell
- ATP-sensitive K+ channels on membrane closes
- depolarisation of cell
- Calcium channels on membrane opens
- Influx of extracellular calcium
- contraction of microtubules
- Insulin released by exocytosis
Insulin is biphasic
- First phase (1st peak)
- within 10-15 minutes of stimulation
- release of preformed insulin
- Second phase (2nd peak)
- lasts up to 2 hours
- release of newly synthesised insulin
Metabolic effects
–Promote glycogen, protein & TG synthesis
Liver cells
- Increases oxidation of glucose (glycolysis)
- Increases glycogen synthesis
- Increases conversion of glucose to fatty acids
- Inhibits gluconeogenesis
- Inhibits glycogenolysis
Muscle cells
- Increases uptake of glucose into cells
- Increases oxdation of glucose
- Increases synthesis of glycogen
- Increase amino acid uptake & protein synthesis
Adipose tissue
- Stimulates uptake of glucose & convert to glycerol
- Increases TG synthesis –> fat storage
- Inhibits lipolysis
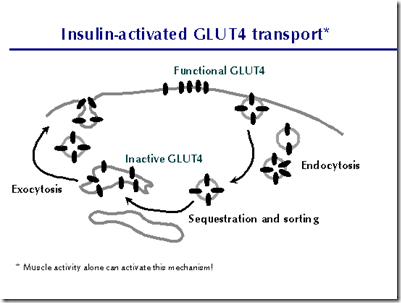
Effect on membrane transport
- glucose: hydrophilic, cell membrane: hydrophobic
- cannot enter by simple diffusion
- facilitated diffusion glucose transporter protein
- Insulin causes muscle & adipose cells to recruit glucose transporters (GLUT4) from intracellular stores to cell membrane
- In liver cells,
- does not promotes facilitated diffusion & uptake
- stimulate glucokinase (for oxidation process)
Mechanism of action
Insulin receptor consists of
- 2 alpha subunit
- binds insulin
- 2 beta subunit
- has tyrosine kinase activity & autophosphorylation site
Insulin binds to alpha subunit of the receptor and activates tyrosine kinase in beta subunit. The tyrosine kinase residues on the beta subunits are phosphorylated. The tyrosine kinase also phosphorylates intracellular proteins like insulin receptor substrate (IRS). Upon phosphorylation of IRS, IRS interacts with other intracellular proteins –> mediating different biological effects of insulin.
Insulin deficiency
- Diabetes mellitus: metabolic disorder characterized by hyperglycemia with disturbances in carbohydrate, protein & fat metabolism. Occurs when mex level of renal tubular reabsorption of glucose is exceeded –> glycosuria.
- urine volume increased due to osmotic diuresis (polyuria)
- leads to dehydration –> increased thirst & polydipsia
- loss in calories –> loss of muscle and adipose tissue –> severe weight loss –> polyphagia
- Increased lipolysis –> increased plasma FA –> B-oxidation in the liver –> increase in ketone body synthesis (hydroxybutyric acid & acetoacetate)–> ketonemia –> increase in plasma H+ (plasma acidity) –> hyperventilation (remove CO2)
- unchecked metabolic acidosis, patient can die in diabetic coma
- Release of K+ from cells –> excreted in urine (dragged by ketone body)
- exogenous insulin given to these patients will cause K+ uptake back into the cell. But can lead to hypokalemia (low blood K+ level)
- Hyperglycemia cause non-enzymatic attachment of glucose to protein molecule (HbA1C)
- Insulin independent tissues like lens & nerves allows glucose to enter freely. Glucose will then be reduced to sortibol. Problems arising from this would be:
- Diabetic cataract
- In nerve cells, sorbitol decreases cellular uptake of myoinositol (decreases the activity of plasma membrane Na/K ATPase). It affects nerve function with hypoxia. Reduced nerve blood flow will lead to diabetic neuropathy.
_____________________________________________________________________
Glucagon
Biosynthesis & structure of glucagon
- 29 amino acids
- 1 polypeptide
- Gene is on human chromosome 2
Preproglucagon –> proglucagon –> glucagon
Effects of glucagon
Liver
- Increases glycogenolysis
- no effect in muscle: does not have glucose-6-phosphatase
- Increases gluconeogenesis
Adipose tissue
- Stimulates lipolysis
Mechanism of action
Glucagon binds to cell membrane receptors and activates adenylate cyclase which increases cAMP. cAMP activates cAMP-dependent protein kinase which increases phosphorylation of specific enzymes/proteins –> biological effects.