Pyogenic meningitis (bacterial)
Location
- brain stem
- cerebellum
- dorsum of brain
Aetiological agents
- Neisseria meningitis
- Strep pneumoniae
- extremes of age
- Anaerobic/microaerophilic streptococci
- brain/epidural abscess
- trauma
- neurosurgery
- Group B streptococci
- neonates/infants
- Staph epidermitis
- intracranial shunts
- Staph aureus
- post operative surgery
- Bordetella pertusis
- children
- Haemophilus influenzae
- children
- E. Coli
- trauma
- surgery
- lumbar puncture
- Listeria monocytogenes
- extremes of age
- immunosuppression
Pathogenesis
- inflammation
- acculumation of pus in subarachnoid space
- interference with CSF flow
- may result in obstructive hydrocephalus
Factors that may bring about meningeal infection
- inhabitants of the nasopharynx
- factors which predispose to blood stream invasion
- disruption of blood-CSF barrier
- Low immunoglobulin & complement levels in CSF
- Organisms with special predilection for the meninges
Clinical presentation
- Pertaining to meningeal irritation
- Systemic effects specific for infecting bacteria
Lab investigations
- Cerebrospinal fluid
- Macroscopic
- CSF pressure increased
- Turbid (cloudy) appearance
- Biochemical
- Protein raised
- Glucose decreased
- Microscopic
- Polymorph neutrophils
- leukocytes increased
- indicating infection
- Gram stain
- for causal bacteria
- Detection of bacterial antigens
- RIA
- ELISA
- Latex agglutination
- Xray
- Chest
- skull/sinuses
Complications
- Cranial nerve palsy
- CN affected: 3, 6, 7, 8
- transient
- Persistent deafness
- unilateral/bilateral
- Cerebral infarction
- physical/mental retardation
- epilepsy
- Persistent coma
- Obstructive hydrocephalus
- accumulation of pus in the subarachnoid space
- interference with CSF flow
Treatment
- Medical emergency
- Rapid clearance of organisms
- Crucial for survival
- Choice of drugs
- Bactericidal drugs active in CSF
- Gram stain as a guide
- Evidence based
Prevention
- Vaccination
_____________________________________________________________________
Types of intracranial infections
- Tuberculous meningitis
- Leptospiral meningitis
- Subdural empyema
- Brain abscess
Tuberculous meningitis
- Causal organism
- Mycobacterium tuberculosis
- Pathogenesis
- variable onset & clinical presentation
- Transmission
- from elsewhere
- associated with miliary tuberculosis
- Lab investigation
- CSF
- protein raised
- glucose decreased/normal
- moderate pleocytosis
- mononuclear cells
- Microscopic
- Ziehl-Neelsen stain of CSF smear
- Acid fast bacilli
- CSF culture
- Culture on Lowenstein-Jensen medium
- revealed typical dry, heaped-up yellow to buff-colored colonies of Mycobacterium tuberculosis
- incubate for 10 days – 6 weeks
- Treatment
- symptomatic
- Anti-tuberculous therapy (MDT)
- Prevention
- TB control programme
- Vaccination
- BCG (very effective)


Leptospiral meningitis
- Causal organism
- Leptospira
- Pathogenesis
- Enter skin/mucous membrane
- Bacteraemia
- Liver
- Kidney
- CNS
- Lungs
- Clinical features
- Liver – jaundice
- Kidney – Uraemia
- CNS – Meningitis
- Lungs – Pneumonia
- Transmission
- Zoonosis
- excreted in urine
- contaminate water/food
- entry into man
- swimming
- consumption
- Diagnosis
- History
- Clinical features
- Serum agglutinin antibody
- Isoloation of leptospirae from
- blood culture
- urine culture
- Treatment
- Penicillin G
- Prevention
- Avoid contact with contaminated environment
- Post exposure prophylaxis
- Doxycycline
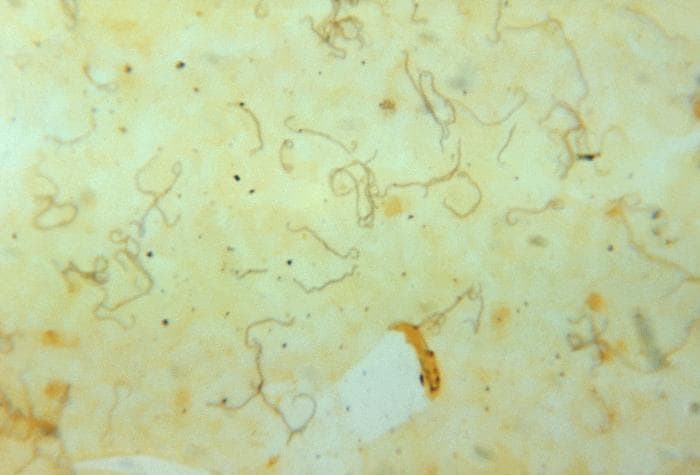
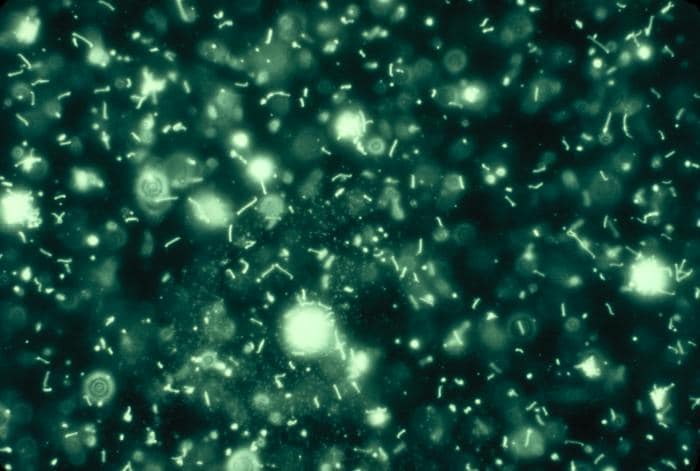
Darkfield microscopy of leptospiral microscopic agglutination test
Subdural empyema
- Causal organism (Polymicrobial)
- Streptococci
- Aerobic
- Microaerophilic/anaerobic
- Staphylococci
- Gram –ve enteric bacilli
- Pathogenesis
- Access
- infection from frontal/ethmoid sinuses
- brain abscess
- septicaemia
- post-surgical
- Pathology
- Collection of subdural pus
- Ischaemic necrossi of affected cerebral cortex
- Clinical features
- Seizures

Brain abscess
- Causal organism (polymicrobial)
- Streptococcus pyogenes
- Microaerophilic/anaerobic streptococci
- Staphylococcus aureus
- Enteric Gram –ve bacilli
- Pneumococci & meningococci
- rare
- Pathogenesis
- focal intracranial suppuration
- Spread
- Blood borne from local foci
- paranasal sinus infections
- localisation at frontal lobe
- middle ear/mastoid infections
- temporal lobe
- cerebellum
- Trauma
- penetrating wounds
- postoperative infections
- Metastatic infections
- lung infections
- bone/dental infections
- endocarditis
- septicaemia
- Encapsulation of liquefied brain & pus by fibroblasts
- Diagnosis
- Primary focus of infection
- Clinical findings
- Imaging studies
- CT
- MRI
- Xray
- EEG
- CSF
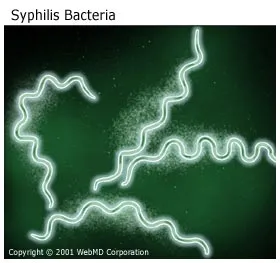
- Causal organism
- Treponema pallidum
- tertiery syphilis
- 10% of untreated infections
- Clinical presentation/Types
- Meningovascular neurosyphilis
- Paretic neurosyphilis
- Tabes dorsalis
- Combination
- Diagnosis
- Clinical grounds
- Past history of syphilis
- Lab investigations
- Nonspecific serological tests
- VDRL
- Rapid plasma reagin test (RPR)
- Specific serological tests
- Treponema pallidum haemagglutination test (TPHA)
- Fluorescent treponemal antibody absorption (FTA-Abs)
- Treponema pallidum immobilisation test
- Treatment
- High dose penicillin G
- Erythromycin
- if allergic to penicillin
- for babies
- Acute meningitis, with bacteriologically sterile cultures (not bacterial)
- Causal organism (neurotropic viruses)
- Picornavirus
- Poliovirus
- Coxsackievirus
- Echo virus
- Mumps virus
- HIV
- Herpes virus
- Herpes simplex virus
- Varicella-Zoster virus
- Clinical findings
- Features pertaining to acute meningitis
- Features pertaining to the specific viral infection
- Viral infection affecting the nervous system
- temporary/permanent paralysis
- death
- Causal organism
- Poliovirus (type 1, 2, 3)
- Transmission
- fecal-oral
- direct contact
- contact-infected secretions
- nose
- mouth
- Clinical features
- Subclinical infection
- Abortive polio
- Nonparalytic poliomyelitis
- Paralytic poliomyelitis
- Complication
- Permanent disability/deformity
- Pneumonia
- Loss of lung/intestinal function
- Lab investigation
- CSF
- CSF pressure increased
- Clear/slightly turbid
- Protein/Glucose normal
- Slight increase in cells
- mainly lymphocytes
- Gram stain –ve
- not bacterial/fungal
- Blood
- specific antibody detection
- blood leucocyte count
- usually normal
- leucopaenia
- Prevention
- General measures
- good sanitation
- Specific measures
- Immunisation
- Preparations
- Inactivated polio vaccine (IPV)
- Oral polio vaccine (IPV)
- may also cause vaccine associated paralytic polio (VAPP)
- Causal organism
- Arbovirus
- JE virus
- Rabies virus
- Herpes virus
- Herpes simplex virus (type 1,2)
- Varicella-zoster virus
- Cytomegalovirus
- most common viral pathogen in AIDs
- Poliovirus
- HIV
- Pathogenesis
- Primary
- direct invasion
- multiplication of virus in brain
- Secondary
- secondary to other viral infection
- post vaccination
- Slow progression, prolonged incubation period
- Causal organism
- JC virus
- Progressive multifocal leucoencephalopathy (PML)
- fatal demyelinating disease
- Measles virus
- Subacute sclerosing panencephalitis (SSPE)
- Self-replicating protein
- Diseases
- Bovine Spongiform encephalopathy (BSE)
- Transmissible Spongiform encephalopathy (TSE)
- Mad Cow diease
- Kuru
- associated with cannabalism
- Creutzfeldt-Jakob disease (CJD)
- variant CJD (vCJD)
- Gertstmann-Straussler-Scheinker syndrome (gCJD)
- Scrapie
- Lab investigation
- CSF
- findings similar to viral meningitis
- Radiography
- CT
- MRI
- EEG
- Brain biopsy
- For HSV encephalitis
- Electron microscopy
- Immunofluorescence microscopy
- PCR
- For HSV encephalitis
- replace brain biopsy
- Transmission
- Zoonosis (infects all warm blooded animals)
- Pathogenesis
- Entry
- via skin/mucous membrane
- inhalation, animal bite, contamination of fresh wound
- Access
- CNS via peripheral nerves
- Spread
- from cell to cell
- Clinical features
- Incubation period
- 1-4 months
- Prodromal manifestations
- hydrophobia
- CNS manifestations
- convulsions
- Death
- CNS/respiratory failure
- Diagnosis
- History
- Clinical manifestations
- Lab diagnosis
- Specimen:
- saliva
- brain biopsy
- Stain & Microscopy
- Negri body
- Immunofluorescent stain
- Seller’s stain
- intracytoplasmic inclusion within nerve cells
- Electrom microscopy
- viral particles
- Treatment
- Antirabies serum
- may/may not be effective
- Supportive
- Symptomatic
- life support mechanisms
- Prevention
- Postexposure in non-immune person
- determine if animal is rabid
- wound debridement
- flush with water
- antiseptics
- Specific treatment
- hyperimmune rabies serum
- rabies vaccine
- Pre-exposure prophylaxis
- rabies vaccine
- Cryptococcus neoformans
- Cryptococcal meningitis
- associated with avians (birds)
- Treatment:
- amphotericin B (with 5-fluorocytosine)
- Lab diagnosis
- Antigen detection in CSF
- ELISA
- Latex agglutination test
- Gram stain & india ink stain of CSF
- yeast cells with typical morphology
- Immunofluorecence stain
- Histoplasma capsulatum
- Disseminated infection
- in immunocompromised person
- Tranmission
- inhalation
- Lab diagnosis
- Silver stain
- Treatment
- amphotericin B
- Coccidioides immitis
- Coccidioidomycosis
- Disseminated infection
- immunocompromised person
- Clincal features
- lung infection
- meningitis
- Causal organism
- Naegleria sp.
- can infect healthy person
- fresh water – swimming
- Hartmanella sp.
- Acanthomoeba sp.
- infects immunocompromised persons
- Plasmodium falciparum
- Toxoplasma gondii
- Lab diagnosis
- CSF
- microscopy for causal agents
- Treatment
- no effective treatment
- high mortality rate
- Sometimes
- amphotericin B
- Eosinophilic meningitis
- Angiostrongylus cantonensis
- ingestion of infective larvae in snails
- No treatment
- Gnathostoma spinegerum
- ingestion of larvae in undercooked fish/seafood
- Treatment: Albendazole
- Others
- Ecchinococcus granulosis
- Taenia solium
- Toxocara cati & canis
- Pathogenesis
- Caused by migrating larvae of these nematodes
- in brain/other tissues
- Life cycle
- not continued
- dead larvae
- Inflammatory response
- Increased eosinophils
- Lab investigation
- History
- Clinical grounds
- CSF
- Eosinophilia (also in blood)
- larvae
_____________________________________________________________________
Neurosyphilis
Aseptic (Viral) meningitis
Poliomyelitis (Infantile paralysis)

Viral encephalitis (Meningoencephalitis/Encephalomyelitis)
Slow virus infections
Prion diseases
Rabies encephalitis

Fungal meningitis

India Ink stain


Protozoal meningoencephalitis
*check parasite atlas
Helminthic infections

