What is pain?
- It is an unpleasant sensation, with a protective function
- Definition:
- unpleasant sensory & emotional experience associated with actual/potential tissue damange
What influences the pain you feel?
- Individual coping strategies
- Attitudes
- Previous pain experience
- Cognitive understanding
- Cultural factors
- Current emotional state
Onset
- Sudden
- Mechanical
- Vascular
- Traumatic
- Toxic
- Gradual
- Infective
- Inflammatory
- Neoplastic
- Degenerative
- Endocrine
- Nutritional
Aggravating/Relieving factors
- Movement
- Respiration
- Ingestion (food)
- Type
- Posture
Character/ Quality of pain
- Dull, aching
- Burning
- Gnawing
- Colicky
- Crampy
- Throbbing
- Stabbing
- Sharp, tearing
- Radiating
- Gripping
- Shooting
- Excruciating
- Sharp lancing
Types of pain
- Sharp/Bright VS Burning/Dull
- Fast VS Slow pain
- A-delta fibres VS ‘C’ fibres
- Withdrawal VS Immobilization
- Cutaneous VS Visceral pain
| Cutaneous | Visceral |
| Sharp | Dull,aching |
| Well-localised | Poorly localised |
| Not associated with ANS symp | Associated with ANS symp |
| Not referred to other site | Freq referred to other site |
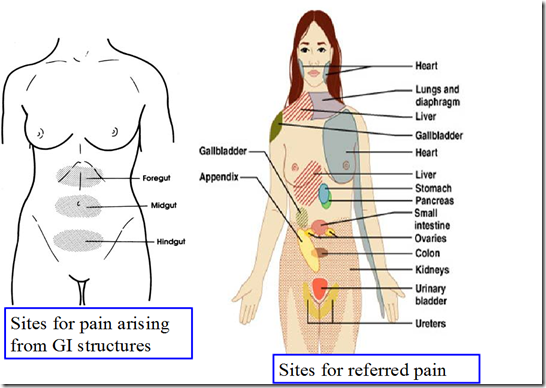
Referred pain
Examples:
- Cardiac pain
- pain in the chest, axilla, arm (T1, T2)
- Gall bladder pain
- pain in the shoulder (C3, C5)
- Pain of appendicitis
- pain in umbilicus
- Ureteric pain
- pain in testes (loin)
- Irritation of nerve endings in meninges and cranial vessels
- headache
Why?
- Dermatomal rule
- Pain is referred to a structure, which is developed from the same dermatome from which the pain producing structure is developed.
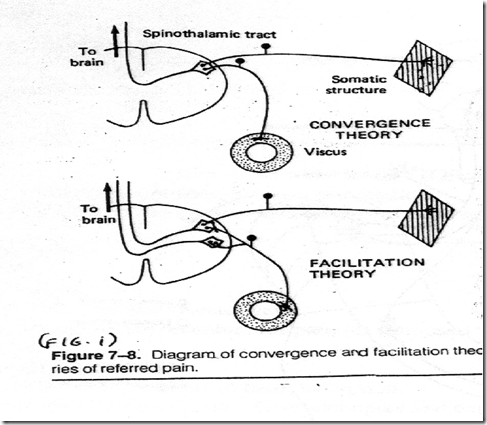
- afferents from skin and visceral structure converge on the projection neuron and impulses generated by them ascend in the same tract – but the brain has ‘learnt’ that impulses usually come from the skin and interpret as such
-
A collateral from the visceral afferent converges on the projection neuron, together with the cutaneous afferent, partially depolarizing the projection neuron - A subthreshold stimulus (eg light touch) from the cutaneous neurone can produce an action potential
_____________________________________________________________________
Postinjury & Neuropathic pain
- Persists while the injury heals
- when the nerves are intact
- Neuropathic pain
- Persists even after the injury has healed
- if the nerves are damaged
- Difficult to manage, resistant to analgesic
- Hyperalgesia
- Minor pain can produce an exaggerated response
- Allodynia
- Innocuous pain such as touch can produce pain
Headache
- Brain itself has very few pain receptors
- but structures nearby have pain receptors
- blood vessels at base of brain
- meninges
- muscles of scalp
- neck & face
- paranasal sinuses
- eyes & teeth
- Mediated by
- mechanical receptors
- eg stretching
- chemical receptors
- eg histamine, serotonin
- Impulses carried by
- 5th & 9th cranial nerves
- by upper cervical cranial roots
- Types of headache
- Chronic/recurrent (benign)
- muscle tension/ tension headache
- Subacute (over days/weeks)
- serious intracranial disease
- encephalitis
- viral/chronic meningitis
- Single, severe episode
- subarachnoid haemorrhage (SAH)
- migraine
- acute meningitis
- Pressure headaches
- headaches of raised intracranial pressure
- intracranial mass lesions displace and stretch the meninges & basal blood vessels
- pain is provoked when these structures are moved physically either by the mass/by raised ICP
- made worse by coughing, straining, sneezing
Pain mechanism/process
- Stimulus
- chemical/mechanical/thermal/biological
- Pain producing substances (PPS)
- kinins
- K+
- histamine
- substance P
- ANG II
- CCK
- NE
- Capsaicin
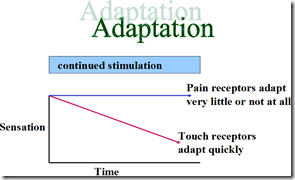
- Receptor
- free nerve endings
- non specific (no adequate stimulus – stimulus for which the receptors are most specific)
- adaptation – very little/none
- Types
- Mechanoreceptors
- in skin
- definite threshold levels
- respond to strong stimuli (pin prick, hot temp)
- fast pain
- warming signal – withdrawal from noxious stimulus
- Polynodal nociceptors
- present in almost all tissues
- no definite threshold level
- respond to tissue damange
- slow pain
- pain causes immobilization of affected part
- to prevent further damage
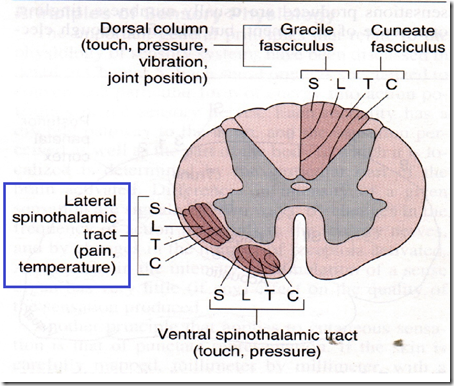
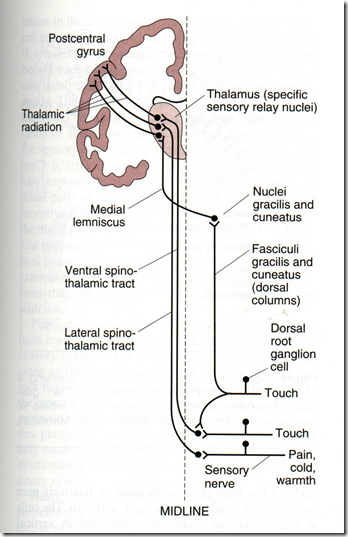
- Sensory nerves (afferents)
- A-delta fibres
- via lateral spinothalamic tract
- together with temperature sense
- C fibres
- via spinoreticulothalamic tract
- Perception
- via thalamus
- Postcentral gyrus (Somatic sensory area 1 – SSA1) & SSA2
- integration centre
- postcentral gyrus (SSA1)
- somatic sensory area 2 (primary & secondary sensory homunculi) / cerebral cortex
Pain pathways
Read from Dr Joachim’s notes on the pathways- Neospinothalamic tract
- Paleospinothalamic tract
1) Neospinothalamic tract (lateral pain system)
- Afferent: A-delta fibres
- To SSA1 & SSA2 of opposite side
- via lateral spinothalamic tract
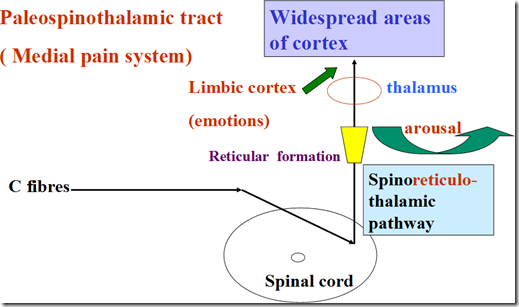
2) Paleospinothalamic tract (Medial pain system)
- Afferent: C fibres
- Goes to limbic cortex (emotions)
- via spinoreticulothalamic pathway
_____________________________________________________________________
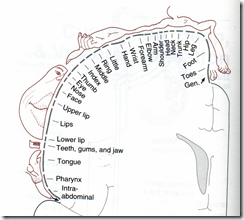
Sensory homunculus
In somatic sensory area 1
- Postcentral gyrus (Broadmann’s area 1, 2, 3)
In somatic sensory area 2
- In Sylvian fissure/lateral sulcus
_____________________________________________________________________
Subcortical perception & affect
- pain can be felt in the absence of the cerebral cortex
- but it is required for discriminative, meaningful & exact interpretation & some of the emotional components
- can feel, but can’t understand it
- the built-in unpleasant affect is mediated by the cingulate gyrus
Role of thalamus
- Understand type, cause, site, amount of pain
- Meaningful interpretation of pain is lost in thalamic syndrome
- damage to posterior thalamic nuclei
- attacks of prolonged, severe, extremely unpleasant pain
- spontaneous/in response to trivial stimuli
Chronic pain syndrome – Phantom limb
- evokes a sensation which is projected to the site of receptor
- eventhough it may no longer exist
- eg. amputated limb
Causalgia
- spontaneous burning pain long after seemingly trivial injuries
- often accompanied by
- hyperalgesia
- abnormally increased pain sense
- allodynia
- Pain from stimuli which are not normally painful
- associated with reflex sympathetic dystrophy
- shiny skin in the affected area
- increased hair growth
- overgrowth of NA sympathetic fibres
- relieved by alpha adrenergic blockade
_____________________________________________________________________
Modulation of pain
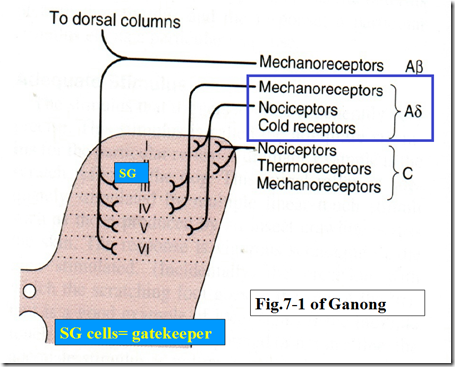
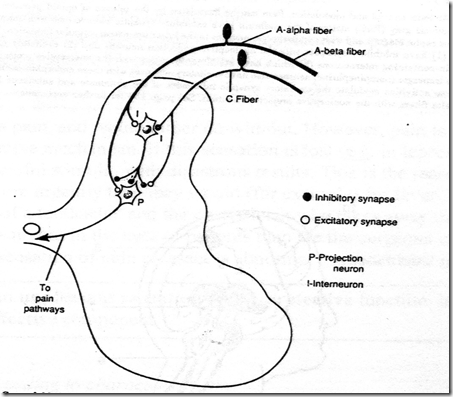
Gatecontrol Theory
- SG cells in dorsal horn
- They inhibit impulse transmission in the projection neuron
- A-delta and A-beta fibres stimulate it
- stimulation of inhibition!
- Therefore: inhibition of impulse transmission
- C fibres inhibit it
- inhibition of inhibition!
- Therefore: no inhibition of impulse transmission
- therefore pain lasts longer
Substances
- Endogenous opioids
- Enkephalins, dynorphins
- a type of analgesic
- NMDA receptor blockers
- esctasy pill
- Analgesics
- narcotics
- NSAIDs
- Opiates
- NMDA receptor inhibitors
_____________________________________________________________________
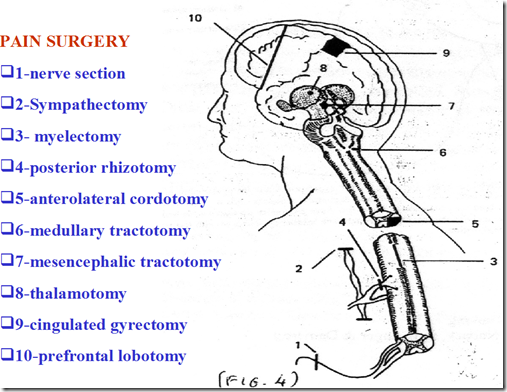
Pain surgery
Extra:
Leave a Reply
Related Posts









Nice job! I am still curious about –
Neuropathic pain, and Trigeminal Neuralgia [Atypical]
Related to shiny skin on lower legs, with hair loss?
I became sutisfied