Tests for peripheral neuropathy
- Electromyography
- measures electrical impulses in muscle at rest & when contracting
- Differentiates between muscle and nerve disorders
- Nerve conduction velocity
- assess the degree of damage in the larger nerve fibres due to myelin loss
- Slow transmission –> myelin damage
- Decrease strength of impulse -> axonal degeneration
- Nerve biopsy
- invasive
- sural nerves (unmyelinated nerve)
- Skin biopsy
- assess damage present in small fibres
- nerve conduction tests cannot assess these
Approach to peripheral nerve diseases
Consider whether the pathology is:
- Primary damage to Schwann cells/myelin
- Acute inflammatory demyelinating polyradiculoneuropathy (GBS)
- Chronic inflmamatory demyelinating polyradiculoneuropath
- Paraprotein neuropathy
- Charcot-Marie-Tooth type 1
- Damage to neuron/axon
- Damage affecting predominantly small unmyelinated fibres
- amyloid
- diabetes mellitus
- HIV
- Affecting all axonal population
- vasculitis
- CMT type 2
- Damage affecting predominantly small unmyelinated fibres
Pathology of demyelination
- Axon damaged
- Neural bodies intact
- Conduction block
- conduction velocity decreases
Patterns of axonal pathology
- Wallerian degeneration
- In transected axon
- distal portion undergoes disintegration & degradation
- Limited recovery & regeneration
- Neuronal body
- chromatolysis
- activation of protein synthesis to help regenerate axon
- chromatolysis
- Examples:
- trauma
- infarction
- diabetic mononeuropathy
- vasculitis
- neoplastic infiltration
- In transected axon
- Distal axonopathy
- Degeneration of axon and myelin starts in the most distal part of the axon
- Axon dies back (retrograde)
- ‘stocking-glove’ sensory
- motor deficit
- Caused by neuronal body pathology
- resulting in inability to sustain the metabolic needs of the axon
- Examples
- drugs
- toxins
- organophosphates
- diabetic polyneuropathy*
- alcohol
- vitamin deficiency
- uraemia
- malignancy
Classification of peripheral neuropathy
By etiology
- Inflammatory neuropathies
- Immune-mediated
- Examples
- Gullain-Barre Syndrome
- chronic inflammatory demyelinating polyradiculoneuropathy
- Infectious
- Examples
- Leprosy (Hansen’s disease)
- Diptheria
- Varicella-zoster
- Examples
- Hereditary
- Examples
- Charcot-Marie-Tooth 1,2 and X
- Examples
- Acquired metabolic & toxic neuropathies
- Examples
- Diabetes mellitus
- vitamin deficiency
- liver disease
- alcohol
- malignancy
- paraneoplastic
- Examples
By site of pathology
- Affecting Schwann cells/myelin
- Acute inflammatory demyelinating polyradiculoneuropathy (GBS)
- Chronic inflmamatory demyelinating polyradiculoneuropathy
- Paraprotein neuropathy
- Charcot-Marie-Tooth type 1
- Affecting the neurons/axons
- Damage affecting predominantly small unmyelinated fibres
- Example
- Amyloid
- Diabetes mellitus
- HIV
- Affecting all axonal population
- Vasculitis
- CMT type 2
_____________________________________________________________________
DEMYELINATING DISEASES
Acute inflammatory demyelinating polyradiculoneuropathy
- General
- Also known as: Guillain-Barre Syndrome
- T-cell mediated immune response & humoral response
- Clinical features
- Rapidly evolving
- Ascending symmetrical weakness
- Areflexia
- Variable autonomic dysfunction
- Mild sensory sign
- Mostly preceded by an acute flu-like illness
- complication of influenzae infection
- Rapidly evolving
- Important features
- Ascending paralysis
- Loss of deep tendon reflexes
- Decreased nerve conduction
- Increase in CSF protein
- Little cell increase
- Infectious agents implicated include
- Campylobacter jejuni
- CMV
- EBV
- Mycoplasma pneumoniae
- Influenzae virus
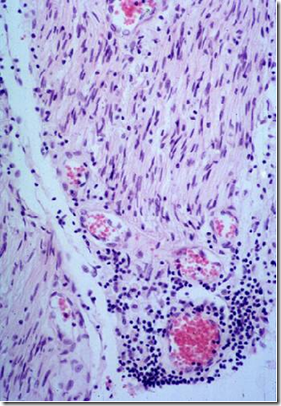
- Microscopic pathology picture:
- Endoneurial lymphocytic inflammation
- macrophage infiltration
- MACROPHAGE mediated DEMYELINATION
- More severe in the nerve roots
- more subtle in the periphery
- Axonal damage when disease is severe
- Electron microscopy
- macrophage penetrating basement membrane of Schwann cells
- Stripping myelin sheath away
- Remyelination can occur
- Endoneurial lymphocytic inflammation
- Plasmapharesis is effective in some cases
Chronic inflmamatory demyelinating polyradiculoneuropathy
- Classical Triad
- Symmetrical proximal & distal weakness
- for more than 2 months
- Loss of large fibre modalities
Loss of deep tendon reflexes - Symmetrical proximal & distal weakness
- Endoneurial inflammation
- Onion-bulb formation in semithin sections
- due to repeated demyelination & remyelination
Hereditary Sensory and Motor Neuropathy (HSMN)
- General
- Also known as Charcot-Marie-Tooth type 1
- Clinical features
- Slowly progressive distal weakness
- Usually begin in childhood
- Muscle atrophy and sensory impairment
- Dominance of distal lower extremities signs and symptom
- Hammertoes
- Pes caves
- high arch
- Nerve enlargement (hypertrophy)
- If nerves palpable and tremors = CMT type 1
- Very slow disease with normal longevity
- Pathology
- Decrease numbers of large & small myelinated fibres
- Onion bulb formation
- Increase in calibre of affected nerves
- nerve hypertrophy
- Axonal form (CMT2)
- no onion bulb, but regenerative axonal clusters
- Genetic mutation of myelin related proteins
Paraprotein neuropathy
- Neuropathy associated with a monoclonal gammopathy
- Incidence
- > 50 yrs
- male
- Clinical features
- Mild slowly progressive symmetrical distal weakness
- Painful with severe sensory loss & paresthesia
- Diagnosis
- Monoclonal IgM with anti-MAG (myelin-associated glycoprotein activity)
- Pathology
- Non-specific myelin & axonal loss
- POEMS syndrome
- polyneuropathy
- organomegaly
- endocrinopathy
- M protein
- skin changes
_____________________________________________________________________
AXONAL DISEASES
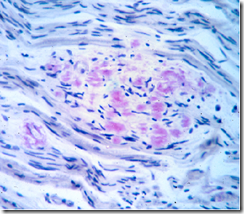
Amyloid neuropathy
- General
- Hereditary/acquired
- Important features
- Small fibre neuropathy
- pain
- temperature
- autonomic dysfunction*
- Small fibre neuropathy
- Clinical features
- Painful dysesthesias
- Bowel & bladder dysfunction
- Impotence
- Orthostasis
- Cardiac & renal abnomalites
- Pathology
- Biopsy abdominal fatpad
- Amyloid deposition in endomerium & vascular wall
- Large myelinated fibres are preserved
- Biopsy abdominal fatpad
Diabetic polyneuropathy
- Cause
- diabetes mellitus
- Most common pattern
- length-dependent axonal sensorimotor polyneuropathy
- Manifest as
- PAIN and PARESTHESIAS
- Clincal features
- Start in distal lower extremities
- longest nerve fibres
- Gait abnormality
- Autonomic abnormality
- ‘diabetic autonomic neuropathy
- Sensory dysfunction distal extremity
- glove & stocking numbness
- weakness of distal lower extremity
- Start in distal lower extremities
- Pathology
- Axonal neuropathy
- Loss of large, small & unmyelinated fibres
- Entirely NON-SPECIFIC
- Pathophysiology
- Nerve ischaemia
- due to diabetic microangiopathy
- poor blood flow
- may easily develop ulceration
- Nerve ischaemia
- Skin biopsy to assess small-nerve fibres
- Easy to perform
- Provides information on small nerve fibres
- not possible with sural nerve biopsy
- nor with routine neurophysiological testing
- Can demonstrate subclinical neuropathy
- eg. in diabetic patients
_____________________________________________________________________
Hansen’s disease
- Causal organism
- Mycobacterium leprae
- Pathology
- In Lepromatous leprosy
- Schwann cells are invaded by the mycobacteria
- Increase in Th2 cytokines: IL3, IL5, IL10
- Increase CD8 cells
- In Tuberculoid leprosy
- active cell mediated immune response
- injures cutaneous nerves
- including axons, schwann cells & myelin
- Increase Th1 cytokines: IL2, IFNγ, TNFβ
- Histology:
- granulomatous inflammation, scanty bacilli
- active cell mediated immune response
- In Lepromatous leprosy
- Clinical features
- Pain fibres affected
- loss of sensation
- Pain fibres affected
Traumatic neuroma
- Non-neoplastic
- Occurs at proximal end of severed nerve
- trauma
- surgery
- Clinical features
- Firm nodule, painful or tender
- Reactive proliferation of schwann cells, axons & fibrous ce
lls
- Reactive proliferation of schwann cells, axons & fibrous ce
- Firm nodule, painful or tender
Tumours of peripheral nerves
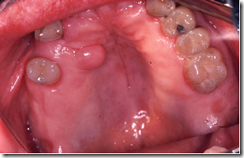
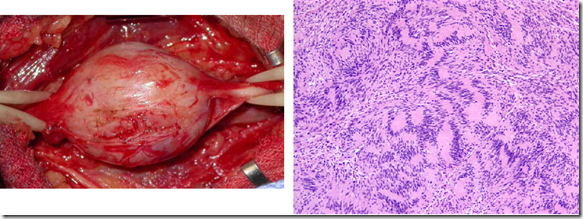
Neurofibroma
- Cutaneous/ in Peripheral nerve
- Plexiform type
- only seen in Neurofibromatosis Type1 (NF1)
- Tumours in NF1 are more likely to become malignant
- Malignant tumours are called
- Malignant Peripheral Nerve Sheath tumours (MPNST)
- Malignant tumours are called
- Histology
- Spindle shaped cells
- Serpentine nuclei
- Schwann cells, axons, fibroblastic cells and perineurial cells are present
Schwannoma
- Arise from Schwann cells
- Histology
- True encapsulation
- Antoni type A & Antoni type B areas
- Verocay bodies
- Multiple tumours seen in NF2
- Benign
- Malignant counterpart is MPNST





We just wrote a small tidbit (sourcing a Harvard study) about using ATP supplementation to lessen or prevent the symptoms of small fiber peripheral neuropathy: http://www.chrisbyrnes.com/2012/01/06/treating-small-fiber-neuropathy-symptoms-with-atp/
Nice