
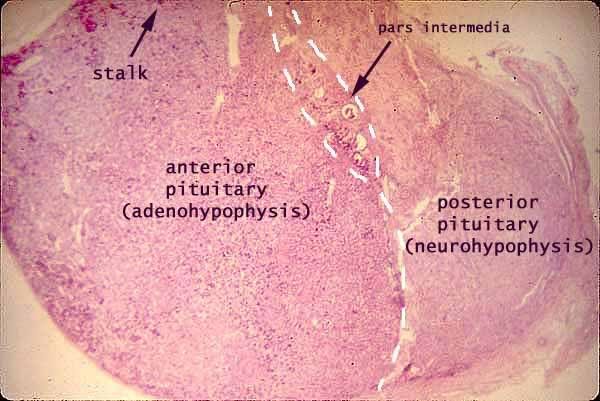
This is a normal anterior pituitary gland histology. Note the bluish colour of the basophils, and pinkish colour of the acidophils.

This is a histology slide of the posterior pituitary.

The brown-stained cells are cells that secrete Growth Hormones – Somatotropes. The cells are stained for immunochemistry evaluation.
_____________________________________________________________________
Pituitary Tumours
**Definition: Neoplasm located in the sella turcica.
Comprises of 10-15% of all intracranial tumours. 27% pituitary glands contain incidental adenomas (very common in people). 1/5 show pituitary abnormality on MRI. Uncommon in children, 2%.
Types of pituitary tumours:
1) Pituitary adenomas from adenohypophyseal – anterior pituitary (most)
2) Pituitary carcinoma (small percentage)
3) Mesenchymal, Neural, Epithelial, Metastases
Pituitary Adenoma
Most common:
1) Prolactinoma – in adults & children
2) ACTH-oma – more frequent in children
Signs & Symptoms – 2 concepts
1) Excessive hormone
- If it’s a funtioning tumour: high hormone level
- Non-functioning tumour: normal hormone level
2) Mass effect
- Intracranial mass: headache
- Loss of normal anterior pituitary hormone production due to compression
- Visual field defect: compression of optic chiasma (tunnel vision)
- Mild hyperprolactinemia (**stalk effect)
Classification
1) Functional – hormone level
2) Histology
3) Ultrastructural
4) Biochemical
5) Imaging
6) Surgical findings
Classification by size (imaging)
Microadenoma – <1cm
Macroadenoma – >1cm
Giant adenoma – >4cm (RARE)

Evaluate growth pattern, expansile, invasive.
Histology

- Monomorphic (just larger/more. No dysplasia)
- Uniform round cells
- Delicate stippled chromatin
- Inconspicuous nucleoli
- Moderate amounts of cytoplasm
- Mitoses: rare
- Ki67 labelling <3% (determine growth)
- Atypical variant
Treatment
1) Surgical – Via transphenoidal approach (minimally invasive)

Only perform surgery when:
- Progressive mass effect (visual loss)
- Hyperfunction (Cushings, acromegaly, hyperthyroid)
- Failure of medical treatment
- Massive acute haemorrhagic necrosis of an adenoma (pituitary apoplexy/Sheehan’s syndrome)

Sheehan’s syndrome – Haemorrhagic & infarcted
2) Medical treatment
Prolactinoma: Give dopamine agonist (inhibits prolactin). Reduces hyperprolactinemia, reduce tumour size.
GH-oma: Somatostatin analogues react with receptors, prevent growth hormone secretion. Does not reduce tumour size.
3) Radiation (Gamma Knife)
Use in:
- Incomplete surgical resection
- Recurrent tumors
- Medically unfit for surgery
- Secretory tumours uncontrolled by other treatment
Complication:
- hypopituitarism
- glioma (tumour of glial cells)
- sarcoma (malignant cancer of CT)
_____________________________________________________________________
Prolactinomas
*Most frequent type

- Cytoplasm weakly acidophilic
- Sparsely granulated/densely granulated
- Dystrophic calcification – pituitary stone
Characterised by: efficiency ( small tumours will also secrete hormone) and proportionality (hormone production proportional to tumour size)
Clinical features:
1) Amenorrhea
2) Galactorrhoea
3) Loss of libido
4) Infertility
These clinical features can also be caused by : prolactinemia, pregnancy, suckling and stress.
Prolactinaemia:
Due to hyperplasia of the lactotroph (secrete prolactin). It can be caused by:
1) Interference with dopamine inhibition (no inhibition of lactotroph)
2) Damage to dopanergic neurons of hypothalamus from trauma (no dopamine)
3) Mass in suprasellar compartment : Stalk effect
Growth Hormone Adenoma
**2nd most common
It will grow to be quite large before it will be clincally symptomatic. It is acidophilic (sparsely/densely granulated)
Immunohistochemistry: GH+ , CK+
Diagnosis:
- High level of growth hormone
- High level of IGF-1
- No suppression of GH with glucose loading
Corticotroph Adenoma

May be basophilic/ acidophilic.
- Usually small
- Most often densely granulated & basophilic
- PAS positive (bcos of carbohydrate content)
Immunohistochemistry: ACTH positive
Clinical features:
- Cushing’s syndrome (collection of signs & symptoms)
- Cushing’s disease (if pituitary tumour)
- Nelson syndrome
-Largely destructive adenoma develop after surgical removal of adrenal glands
-Hyperpigmentation (MSH)
-Mass effect
-No hypercortisolism
 Nelson syndrome
Nelson syndrome
Gonadotroph adenoma
-LH, FSH
Inefficient & variable secretion
No recognisable syndrome
Thyrotroph adenoma
Non-functioning adenomas
-silent
Pituitary Carcinoma
Must show METASTASES.
Suprasellar tumours
Effect: Induced hypo/hyperfunctioning of anterior pituitary / diabetes mellitus / both.
2 main types:
- Gliomas from chiasma
- Craniopharyngiomas (most)
Craniopharyngioma
It is an epithelial tumours (stratified squamous cell epithelia). It represents a bimodal distribution (5-15 years old & 50 years above). Histologically: 3-4cm, encapsulated, cystic/ solid.
2 variants:
- Adamantinomatous
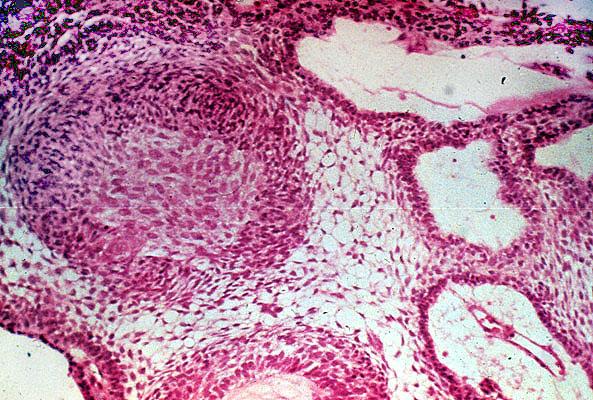
Stratified squamous epithelium
Loose reticulum
Compact lamellar keratin (wet keratin)
Ca
lcification
Chronic inflammation
Cholesterol rich yellowish fluid – machinery oil fluid - Papillary
Solid & papillary sheets of squamous epithelium
No keratin
No calcification
No cysts
No reticulum
Malignant transformation of craniopharyngiomas are RARE, unless there has been radiation.

Howdy! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me.
Nonetheless, I’m definitely delighted I found it and I’ll be book-marking and checking
back often!
Really such a great post!! Provide detailed information about Pituitary Tumors that is helpful for us. Last Monday, I found a website which contains procedure about Pituitary Tumors. I suggest you visit this site http://www.caseysurgicalarts.com/pituitary-tumor-surgery.html