Read from foundation 1 & Dr. Nyunt Wai’s notes!
Synthesis of steroid hormones
- cholesterol
- progesterone
- androgens (C19)
- via aromatase
- Oestrogens (C19)
In male
- testes secrete
- testosterone
- increases LDL, decreases HDL (bad)
- more susceptible to arterosclerosis
- protein sysnthesis
- anabolic steroid: chemical analogue of testosterone
- breast growth, shrinking of testicles
- formation of male internal genitalia
- spermatogenesis
- feedback on LH
- dihydrotestosterone (DHT)
- formation of male external genitalia
- enlargement of prostate
- external virilization
- can be formed from testosterone
- by 5 alpha-reductase type 1/2
- inhibited by finasteride (steroid)
- secreted by prostate into semen
- absorbed thru vaginal mucosa
- if wife pregnant, defective development of male genitalia on male baby. no effect on females.
- adrenal cortex
- DHEA
- androstenedione
Orchidectomy
- Decreased
- facial & body hair,
- muscle mass
- RBC – anemia
- Libido
- Nocturnal erections
- No change
- deep voice. laryngeal change is permanent
Metabolism of steroid hormones
- metabolised in liver
- conjugate with glucoronic acid/sulphuric acid
- becomes water soluble
- secreted in bile
- excreted in faeces
- reabsorbed
- enterohepatic circulation
- excreted in urine
- traces of urinary 17-ketosteroids (24 hour urinary analysis, access androgen secretory status)
If have liver cirrhosis, androgen will be poorly metabolized and remain in body. Androgen will then be converted to oestrogen. Increase in oestrogens which are pooly metabolised will result in feminizing effects (gynaecomastia)
Congenital Adrenal Hyperplasia (CAH)
- Under control of ACTH (not LH)
- act on adrenal androgens
- decreased cortisol production, increased androgen production
- due to 21-beta-hydroxylase deficiency
- cant produce cortisol
- treatment: large doses of cortisol, inhibits ACTH
- Causes early epiphyseal closure in boys –> shorter
- in female: adrenogenital syndrome, masculinization of genitalia
Cervical cycle (different from menstrual cycle)
- Follicular phase
- oestrogen
- cervical glands secrete profuse thin alkaline elastic mucus which dries in aborizing fern-like pattern (cervical smear)
- exfoliated vaginal epithelial cells (vaginal smear)
- increased cornification
- polyhedral cells with pyknotic nuclei
- Breast lactiferous duct growth
- Luteal phase
- oestrogen & progesterone
- cervical glands secrete thick and tenacious mucus
- forms cervical mucus plug
- inhibit ferning effect
- exfoliated vaginal epithelial cells (vaginal cells)
- rolled edges with WBC infiltration
- Breast lactiferous duct growth, lobulo-alveolar growth & retention of fluid
- breat tenderness
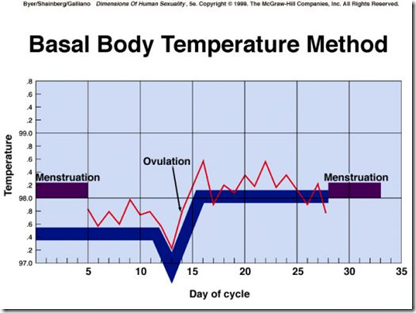
- thermogenic (increase in temperature)
- fertile during this stage
Menstruation
- 4 days after luteolysis
- 10 days after ovulation
- therefore, luteal phase is 14 days (fixed)
Manipulate length of cycles
- Pill
- synthetic oestrogen & progestins
- for contraception
Anovulatory cycles
- 1-2 years after menarche, immature axis
- contraceptive pils
- menopause
Oestrogen
- Increase
- uterine blood flow
- myometrium
- myometrial excitability & contractiligy
- sensitivity to oxytoxin
- if remove ovary (ovariectomy) before 12 weeks of gestation, abortion. Therefore, essential for the maintenance of pregnancy.
- epiphyseal closure
- fluidity of sebaceous gland
- salt & water retention
- Decrease
- bone resorption
- so after menopause, osteoporosis is rampant. increase in bone resorption
- plasma cholesterol, prevents coronary heart disease
Progesterone
- prepares endometrium for implantation
- anti-oestrogen action on myometrium
- decrease excitability
- decrease sensitivity to oxytocin
- Mifepristone: blocks binding of progesterone to it’s receptors
- abortion
Stress can inhibit GnRH production & secretion.
Read from foundation 1 notes: If GnRH secretion is tonic(continous) and not pulsatile, there will be down regulation of GnRH receptors.
- Therefore a woman suffering from oestrogen-dependent breast cancer, to suppress ovarian production of oestrogen by giving IV infusion (not hourly IV injection) because of it’s continuous manner of secretion, GnRH receptors will be less, hence less ovarian function. Same goes to males.
- However, if there is ovarian hypofunction, and oestrogen secretion should be stimulated, an hourly IV injection should be given.
A woman suffering from oestrogen dependent breast cancer, to reduce the effect of oestrogen on tumour cells,
A. Aromatase inhibitors may be given
B. Receptor modulatior like Timoxifen may be given
C. Ovaries may be surgically removed
Gonadotrophin
- Pituitary
- FSH
- LH
- Placental
- hCG
- maintain corpus luteum production of oestrogen & progesterone before placenta is self-sufficient (12 weeks)
- test for pregnancy
- act on same receptor as LH, can be used for undescended testes.


overactive sebaceous glands can lead to more acne and acne scarring if they get infected. ‘
My web blog
http://www.healthmedicinelab.com/canker-sore-on-tongue/