- Deficiency of any of the adrenocorticoid steroid hormones
Hypoadrenalism
- Reduced adrenocortical function
- Deficient synthesis of steroid hormones
- ACTH deficiency – Can’t stimulate the adrenal cortex
Primary Adrenocortical insufficiency
- Disease of the adrenal gland
Acute: Adrenal crisis
Sudden loss of adrenocortical function caused by:
- Bilateral adrenalectomy (as a treatment of cortical hyperfunction & hypertension)
- Septicaemia (from endotoxic shock, meningococcal infection producing hemorrhage, necrotic adrenal cortex).
- Waterhouse- Friderichsen’s syndrome: disease of adrenal gland caused by Neisseria Meningitidis.
- Rapid steroid withdrawal
- Acute stress
- Acute adrenal hemorrhage
Features of adrenal crisis:
- Deficiency of glucocorticoids (Cortisol) & mineralocorticoids (Aldosterone)
- Glucocorticoid deficiency: hypoglycemia, increased insulin sensitivity, vomiting
- Mineralocorticoids: Salt deficiency, hyperkalemia, dehydration
- Altered mental status
- Shock
- Gastrointestinal & abdominal symptoms
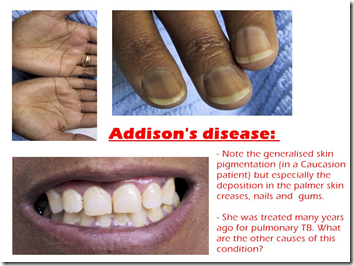
Chronic: Addison’s disease (cortisol deficiency)
Also known as bronze skin disease
- 80% of adrenal insufficiency cases
Bilateral destruction of adrenal cortex (Bilaterally small & irregularly shrunken) caused by:
- *Tuberculosis
- *Autoimmune chronic destruction
- Histoplasmosis
- Metastatic cancer
- Sarcoidosis
- Haemochromatosis
- ACTH receptor insensitivity
Histologic changes reveal features of tuberculosis & histoplasmosis.
Tuberculosis:
- TB thrives in steroid rich environment
- Destroyed adrenal gland.
- Adrenal glands will atrophy and calcify.
Autoimmune disease:
- Anti-adrenal antibodies attached to ACTH receptor sites on adrenal gland, destruction of the receptor sites/ ACTH will not be able to bind to the receptor sites, less cortisol will be formed.
- Associated with other autoimmune diseases – immune thyroid disease
HIV associated diseases:
- Adrenal insufficiency as primary process
Clinical manifestation of Addison’s Disease:
Hyperpigmentation (By ACTH & MSH)
- Non solar exposed skin (creases)
- Dirty hands
- Pigmentation of buccal muscosa & gingiva
- Solar exposed areas – deeply pigmented
- Scars & traumatized area – highly pigmented
Hyponatremia
- Low ACTH, low aldosterone, Na+ loss
- ‘Salt Craving’
Orthostatic hypertension
- Low water retention
- Low blood volume
- Small quiet heart
- Fasting hypoglycemia
- Failure to gluconeogensis
- Increased insulin sensitivity (bcos low glucose)
- Improved glycemic control in diabetic
Androgen deficiency
- Woman: Loss of body hair, decreased libido, amenorrhea
- Man: Sexual dysfunction
Other
- Reduced GFR (low blood volume & low BP)
- Acidosis
- Hyperkalemia (due to low aldosterone)
- Low sodium, chloride & bicarbonate
- Loss of appetite
- Nausea
- Vomiting
- Upper abdominal pain
- Eosinophilia & lymphocytosis
Secondary Adrenocortical insufficiency
Caused by:
- Diminished secretion of ACTH by pituitary gland
- Selective ACTH defiency due to prolonged administration of corticosteroids.
- Panhypopituitarism (low MSH, low ACTH, normal aldosterone due to renin)
Features:
- Lack of stimulation of adrenal gland by pituitary ACTH –> adrenal gland atrophy
- Lack of hyperpigmentation (due to low MSH & ACTH)
- In Primary adrenocortical insufficiency: Decreased blood cortisol results in increased pituitary ACTH production and increased blood β-lipotropin, which has melanocyte-stimulating activity and, together with ACTH, produces the hyperpigmentation of skin and mucous membranes characteristic of Addison’s disease. Thus, adrenal insufficiency secondary to pituitary failure does not cause hyperpigmentation (because in secondary, pituitary itself cannot produce ACTH).
Hypoaldosteronism
- Deficient secretion of aldosterone
- Normal cortisol levels
It is however not due to any defect of the target organ but due to reduced renin (renin-angiotensin-aldosterone system) which can be caused by:
- Congenital defect (enzyme deficiency for renin synthesis)
- Prolonged heparin administration
- Excision of aldosterone secreting tumour (?, unless adrenal cortex function is abnormal as well)
- High blood pressure –> inhibit renin secretion by juxtaglomerular apparatus.
Predominant features:
- Hyperkalemia & metabolic acidosis (due to low Na+ reabsorption)
_____________________________________________________________
Hormonal Deficiency
Summary:
When diagnosing deficiency of hormone, it is a bit more complicated than hypersecretion. Hypersecretion can be easily pointed to a tumour, ectopic tumour or the increase of the releasing and stimulating hormones by the hypothalamus and pituitary gland.
When diagnosing the cause of a hormone deficiency, we have to 1st consider the target organ itself. This will be problems at the PRIMARY level.
- Receptor
- Organ
- Post-receptor
Consider these 3 factors. At the receptor level, it can be due to destruction of the receptor itself (by infection or autoimmune) or insensitivity towards the hormone. At the organ level, it can also be due to destruction of the organ (infection, autoimmune, trauma), the lack of certain enzyme to produce the hormones (especially adrenal steroids) or removal of the organ itself. At the post-receptor level, it can be due to defect in the hormone, therefore it is ineffective.
Secondly, we have to consider the problems of the pituitary gland at the SECONDARY level.
- Receptor
- Organ
- Post-receptor
Using the same factors, at the receptor level, the reasons are the same as mentioned above. If there are problems with the receptor in receiving the hormones from the hypothalamus, then the pituitary gland won’t be able to synthesize their hormones as well, causing a chain effect of not being able to stimulate the target
organs as well. At the organ level, pituitary gland would have been injured or removed. And at the post receptor level, with the same reasons.
TERTIERY level will be the hypothalamus.
- Feedback
- Organ
- Post-organ
Unlike the target organs and pituitary glands, the hypothalamus does not receive hormones for stimulation. However, it receives feedback from the body on the levels of hormones in the body. If a hormone is too excessive, then a negative feedback will inhibit the hypothalamus from stimulating the pituitary gland from secreting more hormones. However, if a hormone is needed, the hypothalamus will be alerted and hence produce the necessary hormones & neural signals to the pituitary. BUT if there is a defect in the feedback mechanism, meaning the hypothalamus might not be able to secrete the necessary hormones to begin with. At the organ level, the hypothalamus might have been removed, or injured. And at the post-organ level, the secretion might be defective and ineffective to stimulate the pituitary gland.
Despite the causes, the general concept is this: If there is decreased stimulation on the target organ, the organ can be wasted and atrophy. Therefore, if a condition is chronic, the atrophied organ may cause permanent damage. Hence, even if there is stimulation, the atrophied organ might not be able to produce the same amount of hormone as the normal organ would.


>I appreciate your post, i learn few things in this post, I have book marked this internet site so ideally I’ll see much more on this subject in the foreseeable future!Disability Products