Recap:
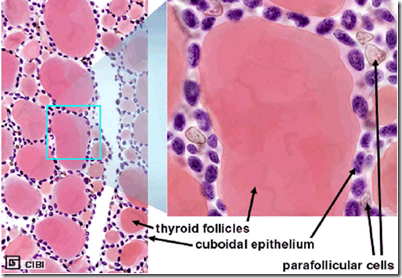
Thyroid follicular cells: Cells surrounding the follicle, there are microvilli projecting into the colloid from the apexes, with abundant endoplasmic reticulum.
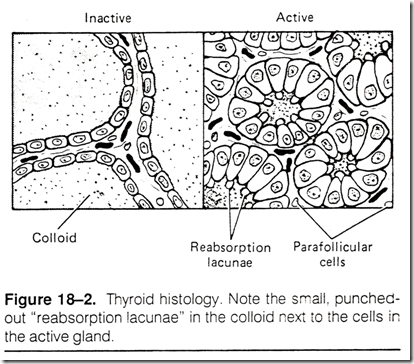
Inactive gland,
- colloid is abundant
- follicles are large
- cells lining the follicle are flat
Active gland,
- follicles are small
- cells lining the follicle are cuboid/laminar
- Edge of cells are scalloped
- forming many small ‘resorption lacunae’
Note the parafollicular cells.
_____________________________________________________________________
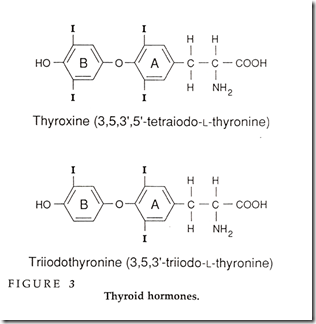
Thyroid hormones
T4
- Major hormone secreted by the thyroid follicles
- 4 bound iodine atoms
- Constructed from the linkage of 2 tyrosine amino acid
T3
- most is formed at the target tissues by conversion of T4 to T3
- 3 bound iodine atoms
- Constructed from the linkage of 2 tyrosine amino acid
Biosynthesis of thyroid hormones
Thyroglobulin
- Contains precursors of T3 & T4
- Large iodinated, glycosylated protein
- Molecular weight of 660k
- Carbohydrate: 8-10% of it’s weight
- Iodine: 0.2-1% of it’s weight, depending on the diet
Iodine
- 70% of iodine in the thyroglobulin are attached to the INACTIVE PRECURSORS
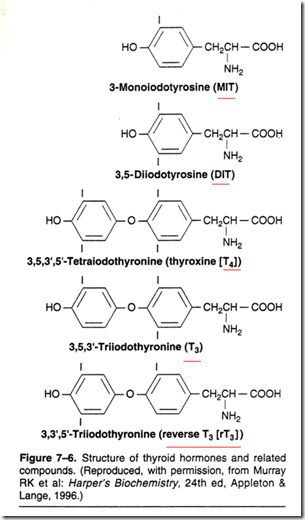
- MIT (monoiodotyrosine)
- DIT (diiodityrosine)
- 30% of iodine in the thyroglobulin are in the IODOTHYRONYL RESIDUES
- T3
- T4
When iodine supplies are sufficient
- T4:T3 = 7:1
Thyroglobulin
- Storage form of T3 & T4 in the colloid
- can stock up for several week’s supply
- advantage of attaching to thyroglobulin
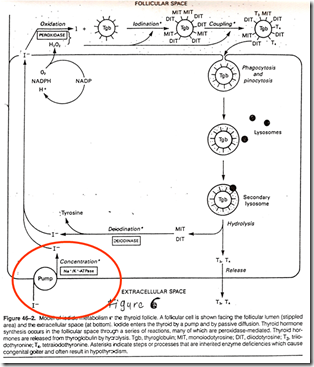
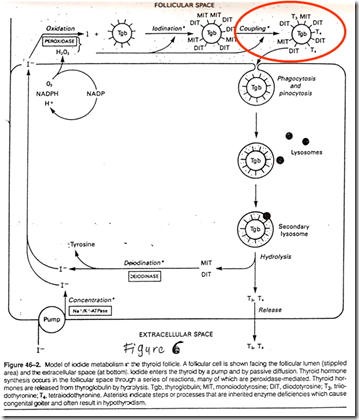
Process of biosynthesis of thyroid hormones
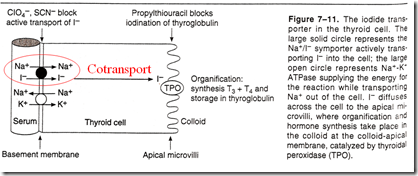
1. Trapping of Iodide (I-)
- The thyroid will be able to concentrate iodide against a strong electrochemical gradient
- Pump Iodine from serum to follicular cell
- The ratio of iodide in thyroid : serum (T:S ratio) = 25:1
- It is an active transport
- I- pump is needed
- Pump is linked to the ATPase-dependent Na+/K+ pump
- This pump is stimulated by TSH
- Requires influx of Na+ as cotransport
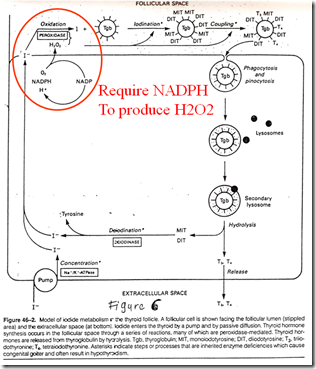
2. Oxidation of iodide
Oxidation of I- involves a heme-containing peroxidase (Thyroperoxidase)
- occurs in the luminal surface of the follicular cell
- a tetrameric protein with a MW of 60k
- Requires H2O2 as an oxidising agent
- H2O2 produced by an NADPH-dependent enzyme
- Resembles cytochrome c oxidase
- H2O2 produced by an NADPH-dependent enzyme
- Antithyroid drugs (thiourea drugs) inhibit oxidation
- thyroid hormone sysnthesis inhibited
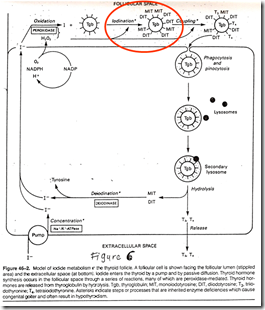
3. Iodination of tyrosine (Organification)
Oxidised I- reacts with tyrosyl residues in thyroglobulin in a reaction that involves thyroperoxidase.
- Iodinate to form MIT & DIT
- 1stly: The 3 position of the aromatic ring is iodinated
- 2ndly: The 5 position is iodinated
- Organification reaction
- Occur in luminal thyroglobulin
- Once iodinated, iodine does not readily leave the thyroid
- Attached to tyrosyl residue in the thyroglobulin
4. Coupling of iodotyrosyls
When the tyrosyls are iodinated, forming iodotyrosyls (MIT/DIT), coupling will occur to form T3 & T4 respectively. This reaction is also catalysed by thyroperoxidase, by stimulating free radical formation of iodotyrosine.
- 2 DIT = T4
- 1 MIT + 1 DIT = T3
- Drugs that inhibit oxidation also inhibits coupling
- The thyroid hormones formed (T3/T4) remain as integral parts of thyroglobulin
- Still attached to thyroglobulin, stored in lumen of follicles until degraded later
5. Hydolysis of thyroglobulin
After stimulation of TSH, there will be marked increase in microvilli (of the follicular cells) on the apical membrane.Thyroglobulin (Tgb) is engulfed by endocytosis and reenters into the follicular cell. (Refer figure above)
The Tgb engulfed will be within a phagosome when in the follicular cell. The phagosome will then fuse with lysosomes to form phagolysosomes. Various acid proteases & peptidases hydrolyses the Tgb into amino acids & iodotyronines.
T3 & T4 are discharged from the follicular cells & subsequently pass thru the basal membrane by facilitated diffusion and enters the capillary lumen.
- The iodine removed from MIT & DIT is scavenged by deiodinase. Iodine can be recycled.
_____________________________________________________________________
Transport of thyroid drugs
- Most T3 & T4 are bound to plasma proteins (99.96%)
- Small unbound free hormones
- Active
- Responsible for biologic activity
- Involved in
- Feedback control
- Tissue action
- Hormone metabolism
- Fecal excretion (out of body)
Plasma proteins:
- Thyroxine-binding globulin (TBG)
- glycoprotein
- Molecular weight 50k
- 100x more affinity than TBPA
- Produced in liver
- Synthesis increased by oestrogens
- pregnancy, birthcontrol pills
- Synthesis decreased by
- androgens
- glucocorticoid therapy
- liver disease
- Thyroxine-binfing prealbumin (TBPA)
- Albumin
- Non specific
- Rapid dissociation rates makes it a major source of carrier of free hormones
***Difference between T3 & T4:
- There are more T4 produced
- There are more free unbound T3
- T4 are more highly bound
- T4 has longer half-life (longer acting)
At target organs,
- deiodination converts T4- T3
- about 80% circulationg T4 converted to T3/reverse T3 (rT3) in the periphery
Reverse T3: A very weak agonist (1% activity of T3) that is made in relatively large amounts in
- chronic disease,
- in carbohydrate starvation
- in fetus
_____________________________________________________________________
Mechanism of action of Thyroid hormones
Thyroid hormone binds to specific high-affinity receptors in the target cell nucleus.
- T3 10x affinity of T4
- T3 3-5x more potent than T4
- T3 less tightly bound to plasma proteins
- T3 binds more avidly to thyroid hormone receptors
Thyroid hormone-receptor complex then binds to DNA & increase the expression of specific genes. The resultant mRNAs then trigger production of various enzymes that alter cell function. The transcription of the growth hormone gene is also enhanced, hence more Growth hormone produced as well.
_____________________________________________________________________
Metabolism of thyroid hormones
1. The thyroid hormones enter the liver and undergo:
- hepatic glucoronidation
- hepatic sulfation
The hormones become more hydrophilic and are excreted into the bile and reabsorbed into the gut.
2. The thyroid hormones enters the kidney & undergo:
- deiodination
The hormones are excreted as glucoronide conjugate in the urine.
____________________________________________________________________
Regulation of thyroid secretion
Regulated by variations in the circulating level of pitutiary TSH
- TRH – TSH – TH
- TSH increased by TRH
- also increased by cold
- TSH inhibited by free T3/T4 (negative feedback)
- also inhibited by stress & warmth
When TSH stimulation is prolonged, thyroid enlarges = Goiter.
- Secretion is pulsatile
- Mean output starts to rise at 9pm
- Peaks at midnight
- Declines during the day
- Peak secretion unrelated to sleep, meals or other pituitary hormones.




Thank you.