Structure & Composition of bone
Structure
- specialized connective tissue
- with minerals within infrastructure
- organic compounds:
- osteogenic cells
- osteoblasts
- osteocytes
- osteoclasts
- Tissue components of bone
- Osteoid (major)
- 30% of total skeleton mass
- Made up of
- Organic matrix
- 90-95% of organic matrix : type 1 collagen fibers
- Ground substance
- ECF
- glycoproteins
- proteoglycans
- chondroitin sulfate
- hyaluronic acid
- Osteocalcin
- a vitamin K dependent protein
- synthesized by osteoblasts at sites of new bone formation
- binds to hydroxyapatite – participate in
- Organic matrix
- Mineral matrix
- Hydroxyapatite crystals
- made up of bone salts (calcium & phosphate)
- crystalline salts deposited in organic matrix
- long, flat plate
- Tightly packed around collagen
- hardens bones
- bones last longer after death
- made up of bone salts (calcium & phosphate)
- Other ions (conjugate to hydroxyapatite crystals)
- Na+
- Mg+
- K+
- CO3- (carbonate)
- Hydroxyapatite crystals
- Osteoid (major)
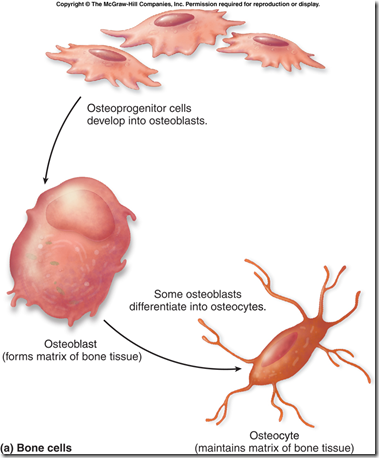
Bone cells (3 types)
- Osteoblasts
- originate from progenitor cells within osteogenic tissue of the bone
- arises from mesenchymal precursor cells in bone marrow
- principal bone forming cell
- while differentiating (to osteocytes)
- acquire PTH & Vitamin D receptors
- surface expression of alkaline phosphatase
- expression of bone matrix protein genes
- type 1 collagen
- osteocalcin
- osteopontin
- others
- Stimulate osteoclast formation and activation
- via cell surface molecule RANKL
- Receptor Activator Nuclear factor Kappa B ligand
- stimulated by
- Vit D
- PTH
- cytokines
- IL-1
- IL-6
- IL-11
- TNF
- originate from progenitor cells within osteogenic tissue of the bone
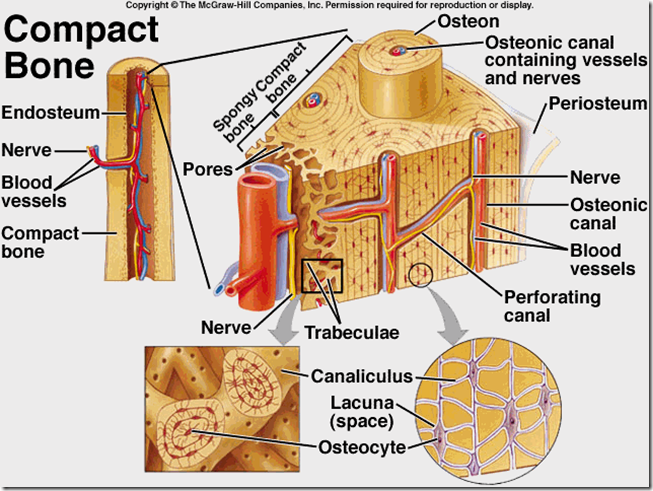
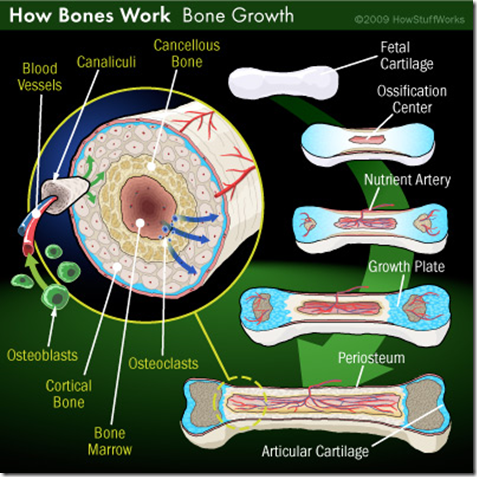
- Osteocytes
- originate from progenitor cells (same as above)
- mature bone cells
- derived from osteoblasts
- occupies lacunae
- remain trapped within the cortical bone during remodelling process
- develops multiple processes – canaliculi
- reach out through lacunae in bone tissue
- communicate with
- nutrient capillaries
- processes of other osteocytes within unit of bone (osteon)
- processes of surface osteoblasts
- acts as cellular syncytium
- permits translocation of minerals in and out of regions of bone removed from surfaces
- sensors of mechanical loading
- provide key signals
- that trigger bone modelling and remodelling
- responsible for osteocytic osteolysis (see below)
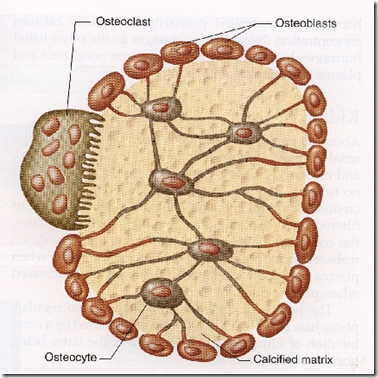
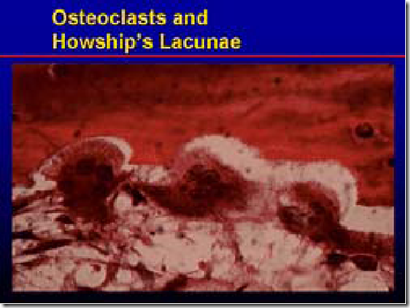
- Osteoclasts
- orginate from mononuclear phagocytic cells (haemopoietic monocyte lineage)
- it is a multinucleated giant cell
- from fusion of several precursor cells
- bone resorption
- during growth and skeletal remodelling
- occupies the surface of bone and erode it
- lies in Howship’s lacunae
- dig a cavity into bone
- at the site of contact with bone, there is a highly folded border – Ruffled border of microvilli
- orginate from mononuclear phagocytic cells (haemopoietic monocyte lineage)
- Bone mineral
- major form
- hydroxyapatite crystals of varying maturity
- minor form
- amorphous calcium phosphate
- occurs in regions of active bone formation
- larger quantity in young bone
- lacks a coherent x-ray diffraction pattern
- amorphous calcium phosphate
- major form
Bone mineralization
- Hydroxyapatite crystals are deposited on the collagen layers to produce lamellar bone
- Mineralization requires (secreted in large amounts by osteoblasts)
- ECF calcium
- phosphate
- alkaline phosphatase
Osteocytic osteolysis
- Canaliculi of osteocytes permits exchange of calcium from the interior of bones to exterior
- to ECF/Blood
- or from exterior to bone
- via breakdown of bone
- Remove calcium from mineral crystals (bone, hydroxyapatite) when plasma Ca2+ level falls
Bone Calcification
- Osteoblasts secrete
- collagen molecules (collagen monomers)
- wire mesh
- proteoglycans (ground substance)
- cement
- collagen molecules (collagen monomers)
- Collagen monomers polymerize to form collagen fibers
- mix with ground susbstance
- forming osteoid
- cartilage like material
- mix with ground susbstance
- Calcium salts deposited in osteoid
- Osteoblasts entrapped in osteoid
- forming osteocyte
- Calcium salts precipitate on the surface of collagen fibers
- Form hydroxyapatite crystals
- Why is hydroxyapatite not formed in normal tissues?
- Calcium & phosphate in plasma is greater than those required to precipitate
- Inhibitors present in all tissues
- Pyrophosphate is inihibiting precipitation of hydroxyapatite in normal tissue
- If pyrophosphate absent, will have precipitation of calcium in non osseous tissue
- in arteriosclerosis
- in old blood clot
- In bone, osteoblasts secrete substances to inhibit pyrophospahte
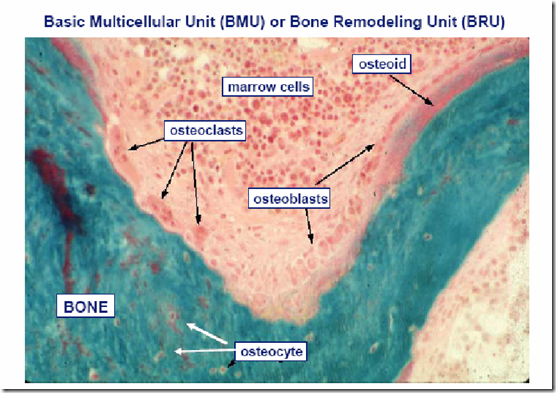
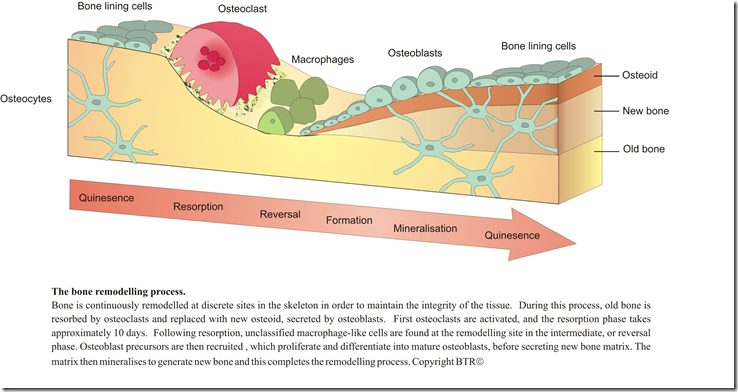
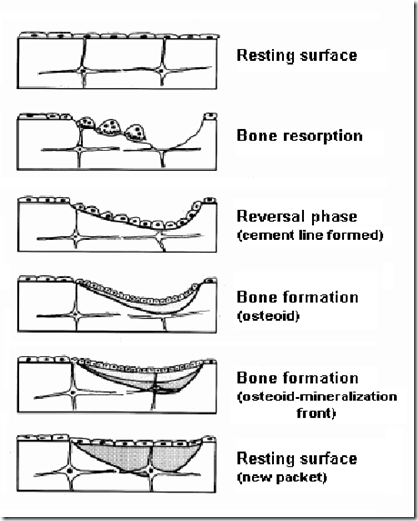
Bone remodelling
- Bone resorption & bone deposit
- at the surface of periosteum & endosteum
- large volumes of bones are removed and replaced
- continuous process
- completion of full remodelling cycle lasts 6 months
- except for growing bones, rate of deposition = absorption
- Does not absolutely require hormones
- but influences remodelling – like PTH
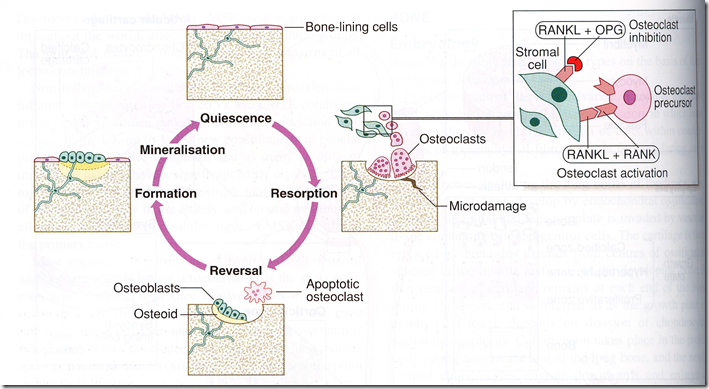
- Bone remodelling unit/ Basic molecular unit (BMU)
- osteoblasts
- osteoclasts
- macrophages
- Bone remodelling process initiated by osteoclasts
- Bone resorption
- by osteoclasts
- forms an adhesive ring – seals off an area
- develops an elaborately invaginated plasma membrane structure – Ruffled border
- Ruffled border villi secretes:
- Citirc acid & lactic acid
- from mitochondria & secretory vesicles
- dissolves bone mineral/salts
- Proteolytic enzyme/proteases (cathepsin K)
- breaks down bone matrix
- Citirc acid & lactic acid
- products endocytosed by osteoclasts and released into the interstitial fluid/blood
- bone matrix
- crystals
- Ruffled border villi secretes:
- releases IGF-1 from bone matrix
- stimulates osteoblast proliferation and differentiation
- after osteoclasts done the resorption
- macrophages phagocytose debris of old bone
- clears the site before bone formation takes place
- by osteoclasts
- Bone formation
- to increase bone strength and to repair injured bone
- new bone deposits by osteocytes
- Factors involved
- local concentration of calcium & phosphate
- regulated by
- PTH
- Vit D
- helps to maintain intestinal absorption of minerals and ensure adequate supply of calcium & phosphorus
- Calcitonin
- regulated by
- matrix proteins
- alkaline phosphatase
- local concentration of calcium & phosphate
- goes to site of resorption when osteoclasts release IGF-1 from bone matrix
Regulation of bone remodelling
Regulation of bone remodelling
- Calcium homeostasis in blood (by hormones)
- Parathyroid hormone (PTH)
- both resorption and formation
- increases proliferation of osteoclasts
- activates already existing osteoclasts
- increases bone resorption
- hyperparathyroidism
- increased osteoclastic activity
- xray – extensive decalcification
- multiple fractures of the weakened bones from slights trauma
- hyperparathyroidism
- PTH receptors in osteoblasts only. Osteoclasts have none.
- Active form of vitamin D (DHCC)
- promotes bone calcification
- increased absorption of calcium & phosphate from the intestines
- enhanced mineralization of bone
- promote development of osteoclasts from precursor cells (act on bone cells)
- vitamin D receptors in both osteoblasts and osteoclasts
- Calcitonin
- inhibits osteoclastic activity
- decreases formation of new osteoclasts
- inhibits bone resorption
- increases bone deposition
- Oestrogen
- slow bone resorption
- decreases the formation of osteoclasts
- oestrogen deficiency (menopause)
- activation of new bone remodelling sites
- exagge
ration of imbalance between bone formation and resorption - increases osteoclast recruitment and activity
- increases apoptosis of osteoblasts
- increases remodeling at trabecular bone (vertebral fractures common)
- oestrogen deficiency (menopause)
- Parathyroid hormone (PTH)
- Mechanical & gravitational forces acting on the skeleton
- By RANKL – ligand
NETT EFFECT
- Bone resorption
- PTH
- osteoblast also secretes IL-6 – more resorption
- inhibits collagen synthesis by osteoblasts
- DHCC
- both PTH & DHCC stimulate osteoblasts to secrete [M-CSF] & RANKL that causes osteoclast precursor cell proliferation
- then differentiate into osteoclasts
- fuse to form multinucleated osteoclasts
- PTH
- Bone formation
- oestrogen
- slows down resorption
- oestrogen
- Inhibit bone resorption
- Calcitonin
- Osteoclast activation
- RANKL + RANK
- Osteoclast inhibition
- RANKL + OPG
Osteon (Haversian system)
Elongated tube of bone matrix with concentrically arranged lamellae of bone surrounding a canal containing blood vessels, nerves and lymphatic. The canal is lined by endosteum.
Haversian canals via Volksmann’s canal, communicates with:
- one another
- periosteum
- marrow cavity
Volkmann’s canal:
- no lamellae around it
- lined by endosteum
Arrangement of collagen fibers – gives extra strength (withstand torsion stress)
- In a particular lamellae
- parallel and run in one direction
- In adjaacent lamellae
- run in opposite direction
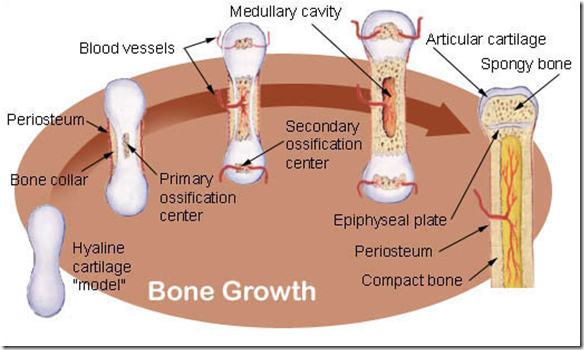
Ossification/Osteogenesis
Refer foundation 1 notes
Starting from foetal skeleton, if it consist of:
- Fibrous membranes
- undergo Intramembranous ossification
- skull cap and clavicle
- fibrous connective tissue membrane have messenchymal cells
- differentiate into osteoblast forming ossification center
- secretes osteoid
- forming non-calcified bone
- blood vessels grow into osteoid
- osteoblasts become osteocytes
- osteoid calcified
- covering messenchyme vascularize and form periosteum
- external compact bone formed
- internal spongy bone formed
- Hyaline cartilage
- undergo Endochondral ossification
- All bones except skull cap and clavicle
- bone collar formation
- cartillage calcified
- then destroyed
- periosteal bud invades (blood vessel)
- osteoblasts reach the center
- via the blood vessels
- osteoid formed
- medullary cavity formed
- osteoid calcified
- primary center – diaphysis
- secondary center – epiphysis
Bone growth
- Growth in length (at adulthood, cartillage cell growth stops and epiphyseal plate becomes thinner & disappear)
- Growth zone
- cartilage cells multiply (mitosis)
- Transformation zone
- cartilage cells enlarge
- matrix calcified
- cartilage cells die
- Osteogenic zone
- osteoblasts secrete osteoid
- osteoclasts remove the calcified cartilage
- Growth in width
- periosteal osteoblasts form new bone on the surface
- increases width
- endosteal osteoclasts remove bone from within
- maintains marrow cavity
Bone repair
- Blood clot forms (hematoma)
- bone cells die
- dead tissue removed
- Fibroblasts invade
- collagen and cartilage formed (soft callus)
- Osteoblasts invade
- Cartilage removed
- replaced by bone (bondy callus)
- Excess bone is removed
- Bone is remodelled





สุดยอดเลย ชอบ
its well and clearly elaborated,easly understandable,well documented,conteined everything,i appreciate it.
This was well written all the key points of the topic were covered with right amount of depth and breadth
Thank you, this cleared up some missing pieces to the puzzle.
thorough presentation, thanks
very well prepared, clear and nice keep on please