Read from Dr. Annie’s notes!
Disorders of development
- Supernumerary nipples/breast
- multiple
- Accessory axillary breast tissue
- Congenital inversion of nipples
- Macromastia/Micromastia
Inflammations
- Acute mastitis
- lactating period
- due to formation of cracks & fissures in the nipple during lactation
- Staph aureus, strep
- localized area of acute inflammation
- pain
- serous fluid
- single/multiple abscesses
- drainage required
- extensive necrosis
- some cases
- Periductal mastitis
- Mammary duct ectasia
- Fat necrosis
- focal necrosis of fat tissue
- due to trauma
- present as breast lump
- ill defined, gray white, firm, nodule
- may be mistaken as carcinoma
- microscopic:
- necrotic fat cells
- foamy macrophages
- inflammatory cells
- foreign body giant cells
- calcification
- mammography might be misleading due to calcification
- Granulomatous mastitis
- Silicone breast implants
- can cause giant cell reaction
- siliconoma – leakage to silicone
Adenoma: increase in acini in lobules
Ductal epithelial hyperplasia: increase in ductal lining epithelial cells
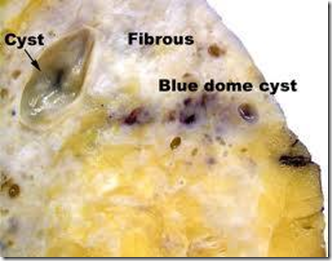
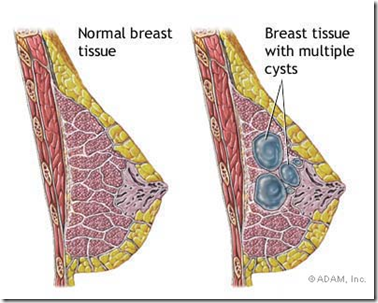
Benign Fibrocytic Change
- Def: Exaggeration & distortion of cyclical breast changes related to menstrual cycle
- 2 types
- Non proliferative
- cystic dilatation of ducts & fibrosis
- metaplastic changes (epithelial)
- Proliferatuve
- Ductal epithelial hyperplasia (ducts & lobules)
- Sclerosing adenosis
- Gross
- Blue-domed cyst
Tumours
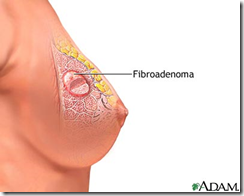
Benign Tumours (will never become malignant)
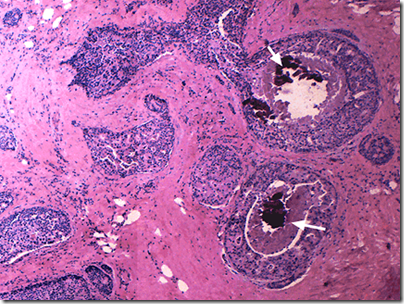
Image: Benign Fibroadenoma
- Benign fibroadenoma
- most common benign tumour
- young
- multiple & bilateral
- upper outer quadrant
- fibrous & glandular tissue
- Gross:
- spherical nodule
- well circumscribed
- freely movable
- vary in size (less than 1cm-15cm)
- Microscopic
- fibrous capsule
- proliferation of both duct & periductal connective tissue
- connective tissue: fibromyxomatous stroma
- Duct, 2 growth patterns
- Pericanalicular pattern (round/oval duct)
- Intracanalicular pattern (slit-like duct)
- Benign tubular adenoma
- Benign ductal papilloma
- Phyllodes tumours
- Arise from intralobular stroma
- Classification
- benign
- low grade malignant
- high grade malignant
- Changes suggest malignant potential
- increased cellularity
- high mitotic rate
- nuclear pleomorphism
- stromal overgrowth
- infiltrative borders
Phyllodes tumour: alot of clefts slits, leaf like structure
Malignant tumours
No oestrogen (non functioning ovaries) will not develop breast cancer! It is a hormone dependent disease
Risk factors:
- early age of menarche
- early age of first full term pregnancy
- hereditary
- race & socioeconomic status
- hormonal – oestrogen exposure
- exogenous hormones
- radiation exposure
- carcinoma at other breast
- endometrial carcinoma
- atypical duct hyperplasia
- obesity
- breastfeeding decreases risk!
Hereditary breast cancer
- Autosomal dominant
- Gene mutation of tumor supressor genes
- BRCA1: risk of ovarian cancer
- BRCA2: risk of male breast cancer
- Sporadic tumours
- Other genes
- p53
- PTEN
Precursor lesions (predispose to breast carcinoma)
- Intraductal proliferative lesions
- atypical ductal hyperplasia
- ductal carcinoma-in-situ (DCIS)
- neoplastic
- limited to ducts & lobules by basement membrane
- myoepithelial cells preserved
- increased epithelial proliferation
- no capacity for nodal/systemic spread
- cant metastasize
- tendency to progress to invasive breast cancer
- not life threatening
- 3 grades (based on cytologic & nuclear characteristics)
- low
- intermediate
- high
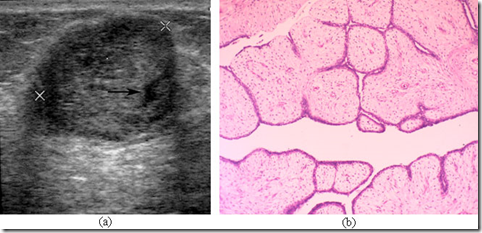
- Subtypes (histological architecture)
- Comedo type (with central necrosis)
- Papillary
- Micropapillary
- Cribiform
- Solid
- florid
- lobular neoplasia/atypical lobular
Image: Comedo ductal carcinoma-in-situ
Paget’s disease of the nipple
- Eczematous nipple
- dermatitis
- Malignan
t cells - from DCIS**
- extend within the duct system into the nipple skin
- Invasive ductal carcinoma and DCIS are the most common underlying malignancies associated with Paget disease.
- When a mass is palpable, invasive carcinoma is common, whereas in the absence of a mass, ductal carcinoma in situ often is encountered
- characterized by large PAS-positive cells with pale cytoplasm and prominent nucleoli
- Paget disease may be found in the vulva in postmenopausal females.
Breast carcinoma
arise from terminal duct lobular unit
Invasive breast carcinoma
Image: Stellate shape of invasive ductal carcinoma
- 2 major categories (based on cytoarchitectural features)
1) Invasive ductal carcinoma
- Subtypes
- medullary carcinoma
- mucinous carcinoma
- tubular carcinoma
- most common breast cancer
- Above 40 yo
- Macroscopic:
- irregular
- stellate outline
- nodular
- firm/hard on palpation
- Gritty feel when cut
- Cut surface: grey-white with yellow streaks
- non mobile
- Microcopic
- tumour cells in cords, clusters or trabeculae
- invades stroma
- solid/synctitial infiltrative pattern
- glandular differentiation manifest as tubular structures
- pleomorphic nuclei
- prominent nucleoli with abundant cytoplasm
- mitotic activity
2) Invasive lobular carcinoma
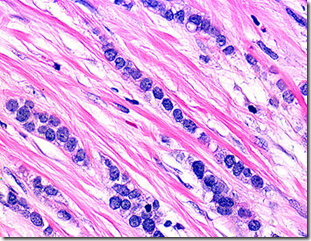
Image: infiltrate stroma in single file
- invasive carcinoma associated with lobular carcinoma-in-situ
- composed of non-cohesive cells
- individually dispersed/arranged in single-file linear pattern
- in a fibrous stroma
- Bilateral (from contralateral/other breast)
- Microscopic
- Proliferation of small cells
- lack cohesion
- individualy dispersed through fibrous tissue
- concentric pattern around normal ducts
- targetoid appearance
- Loss of e-cadherin experssion
- non adhesive
- immunihistrochemistry staining
_____________________________________________________________________
Nipple discharge
Seen in
- Duct ectasia
- thick cheesy
- Periductal mastitis
- premenopausal woman
- serous
- greenish
- bloody
- Benign breast disease (intraductal papilloma)
- postmenopausal woman
- bloody
- serous
- cloudy
- Carcinoma
- old age
- serous
- bloody
- waxy
- associated with palpable mass
3 good prognosis tumours
- medullary carcinoma
- mucinous carcinoma
- tubular carcinoma
Grading of tumour (done for all invasive tumour)
Using the modified Bloom & Richardson method
Based on:
- Nuclear pleomorphism
- Tubule formation
- Mitotic count
Prognostic factors
- Lymph node status
- Tumour size
- Histological type & grade (Bloom & Richardson)
- Hormone receptor status
- Her 2 neu expression
- Distant metastasis
Prognosis bad in pregnancy & men.
Predictive factors ( for response to specific therapy)
- Oestrogen receptor (ER) status
- whether tumour sensitive to oestrogen
- needs oestrogen to survive
- Progesterone receptor (PR) status
- needs progesterone
- Her2/neu
Lab tests done on tumour cells using immmunohistochemistry, ELISA, FISH etc.
Diagnosis
- Clinical signs & symptoms
- Mammography
- Ultrasound
- Biopsy
- FNAC
- Excisional biopsy
- Surgery
- with or without axillary lymph node
_____________________________________________________________________
EXTRA: CASE FILES PATHOLOGY
INTRODUCTION
A 60-year-old woman seeks medical attention for soreness and oozing from the nipple of her left breast. She denies trauma to the breast. On physical examination, there is fissuring and ulceration of the areola and nipple. Biopsy of the breast is performed, and the skin of the nipple is shown in Figure 18-1.
· What is the most likely diagnosis?
· What is the clinical significance of this finding?
ANSWERS TO CASE 18: Paget Disease of the Breast
Summary: A 60-year-old woman complains of soreness and oozing from the nipple of her left breast. On examination, there is fissuring and ulceration of the areola and nipple. Biopsy of the breast skin shows large periodic acid-Schiff (PAS)-positive cells with pale-staining cytoplasm within the epidermis.
· Most likely diagnosis: Paget disease of the breast.
· Clinical significance of this finding: Underlying adenocarcinoma of the breast is often present.
CLINICAL CORRELATION
Introduction
This patient presents with many of the typical clinical symptoms of Paget disease. Paget disease is a rare form of breast cancer that occurs in approximately 1 percent of all breast cancer patients. Patients usually present with symptoms in the sixth decade of life, similar to other common forms of breast cancer. Initial symptoms include erythema and mild eczematous changes of the nipple skin. Scaling and flaking of the nipple may advance to crusting, skin erosion, and ulceration with exudation or frank discharge. A patient also may have pruritus, tingling, burning, pain, or hypersensitivity around the skin lesion. About 40 to 50 percent of all Paget skin lesions have an underlying breast mass.
The differential diagnosis for patients with scaling skin and erythema of the nipple-areolar complex includes eczema, contact dermatitis, postradiation dermatitis, and Paget disease. The presence of bilateral eczematous changes on the nipple-areolar complex is seen more commonly with eczema and contact dermatitis but can occur with Paget disease. Eczema often involves the areola, sparing the nipple (rarely seen with Paget disease). Patients with a history of radiation treatment may have
postradiation dermatitis. Because of the eczematous initial appearance of Paget disease, patients often are started on topical steroids or antibiotics, with transient improvement of symptoms, delaying the diagnosis by an average of 6 months.
Paget disease of the breast invariably has been associated with underlying ductal carcinoma in situ and less commonly with invasive ductal carcinoma. Reports have cited the incidence of underlying carcinoma as being as high as >99 percent. Traditionally, Paget disease has been treated with mastectomy; however, recent reports have shown that more conservative treatment may be possible for select patients. A patient’s prognosis is dependent on the extent of the underlying carcinoma and the stage of the disease, similar to that of females with other types of breast cancer.
Approach to Paget Disease and Ductal Carcinoma in Situ
Definitions
Ductal carcinoma in situ:Considered a malignant lesion with dysplastic cells of the breast ducts that do not invade beneath the basement membrane.
Paget disease of the nipple: A rare type of breast cancer that presents as a scaly red crusty lesion of the nipple or areola.
Discussion
When one is evaluating a patient with a breast lesion, carcinoma must always be considered. The risk of breast cancer is dependent on many factors, such as age, family history, and the specific characteristics of the lesion in question. Many breast cancers can be localized with aid of mammogram screening before symptoms or lesions are clinically apparent. Several clinical features are common to all invasive cancers of the breast, including a fixed position, retraction and dimpling of the skin or nipple, metastases through lymphohematogenous routes with a pattern of nodal spread influenced by the location of the tumor, and distant metastases to any organ of the body.
The diagnosis of Paget disease often is delayed because of its eczematous appearance, and this delay can lead to a diagnosis at advanced stages. When patients present with symptoms suggestive of Paget disease, a diagnosis should be attempted with scrape cytology, superficial epidermal shave biopsy, a 2-mm punch biopsy, a wedge incisional biopsy, or rarely nipple excision. An ideal specimen contains adequate epidermis to provide Paget cells and lactiferous ducts. The histologic hallmark finding for Paget disease is the presence of Paget cells in the epidermis of the nipple; these cells are large with pale-staining cytoplasm and nuclei with prominent nucleoli. Various stains for mucin, epithelial membrane antigens, and low-molecular-weight keratins further characterize these cells. Paget cells usually are located between the normal keratinocytes of the nipple epidermis and the basement membrane. The keratinocyte layer frequently is disrupted, allowing serous fluid to seep through, causing the characteristic crusting and scaling of the nipple skin. Paget cells do not invade through the dermal basement membrane and therefore are a form of ductal carcinoma in situ.
Noninvasive (in situ) intraductal carcinomas account for about 20 to 30 percent of carcinomas of the breast and today are detected more frequently with the use of mammography. This malignant population of cells lacks the ability to invade through the basement membrane and thus is incapable of distant metastasis. These cells can spread throughout the ductal system and may spread up the main duct and into the nipple skin, resulting in the clinical appearance of Paget disease.
Invasive ductal carcinoma is the most common type of breast cancer, accounting for 65 to 80 percent of all mammary cancers. There is usually a marked increase in dense, fibrous tissue stroma, giving the tumor a hard consistency. On gross examination, the tumor averages 1 to 2 cm in size and has a stony-hard consistency. The tumor consists of malignant duct lining cells diposed in cords, solid cell nests, tubules, and glands. The cells invade the connective tissue stroma and frequently invade perivascular and perineural spaces.
COMPREHENSION QUESTIONS
[18.1] A 65-year-old woman complains of itching and scaliness of the right breast nipple area. A 1-cm palpable mass is felt underlying the skin. A biopsy confirms Paget disease. Which of the following is likely to be an association?
A. Infiltrating ductal carcinoma
B. Lobular carcinoma in situ
C. Invasive lobular carcinoma
D. Intraductal papilloma
[18.2] The microscopy of the biopsy of this patient [18.1] most likely demonstrates which of the following?
A. Fibrovascular cores of tall columnar cells extending into ducts
B. Large PAS-positive cells with pale-staining cytoplasm and nuclei with prominent nucleoli
C. Tissue with increased stromal cellularity and cytologic atypia and a leaflike architectural structure
D. Well-formed tubules lined by a single layer of well-differentiated cells
[18.3] What is the most common location for extramammary Paget disease?
A. Liver
B. Lung
C. Kidney
D. Penis
E. Vulva
ANSWERS
[18.1] A. Infiltrating and in-situ ductal carcinomas are the most common underlying malignancies associated with Paget disease.
[18.2] B. Paget disease is characterized by large PAS-positive cells with pale cytoplasm and prominent nucleoli. When a mass is palpable, invasive carcinoma is common, whereas in the absence of a mass, ductal carcinoma in situ often is encountered.
[18.3] E. Paget disease may be found in the vulva in postmenopausal females, with symptoms similar to those of Paget disease of the breast. The same appearance of the Paget cells is noted; however, the risk of underlying adenocarcinoma is far less (about 3 to 5%) with vulvar disease.
PATHOLOGY PEARLS
· Paget disease consists of a scaly red oozing pruritc skin lesion of the nipple, which on biopsy reveals large PAS-positive cells with pale cytoplasm and prominent nucleoli.
· Females with Paget disease of the breast often have an underlying carcinoma.
· The most common type of invasive breast cancer is invasive (infiltrating) ductal carcinoma.



its awesome lecture notes