Cerebrovascular accident (Stroke)
- Described by the side of the brain affected
- not the side of the clinical signs
- Eg. left cerebral infarct leads to right hemiparesis
and dysphasia
Types of stroke
- Infarction
- embolic
- hypotensive
- Haemorrhage
- aneurysm
_____________________________________________________________________
Revision of basic anatomy of the brain
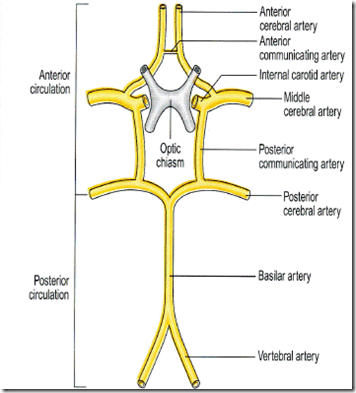
Vascular supply of the brain
- Anterior from
- common carotids
- internal carotids
- then form the Anterior and Middle cerebral arteries.
- Posterior from
- vertebral arteries
- merging into the basilar artery
- forming the Posterior cerebral arteries
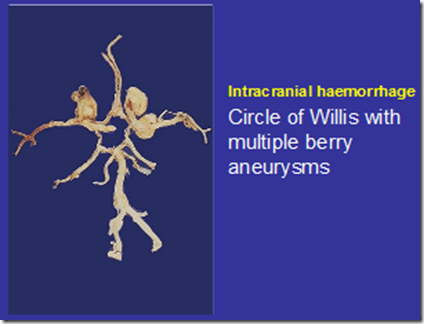
Circle of Willis
- connection of the anterior and posterior circulations around the optic chiasma
- Consist of:
- Anterior communicating artery
- 2 anterior cerebral arteries
- 2 internal carotid arteries
- 2 posterior communicating arteries
- 2 posterior cerebral arteries
Gross functional anatomical areas of the cortex
Arterial territories and functional areas:
- Anterior cerebral arteries
- primary motor cortex
- primary somatosensory cortex (hips to feet)
- Middle cerebral artery
- frontal primary motor cortex (hips to head)
- parietal cortex primary somatosensory cortex (hips to head)
- temporal lobe (auditory and olfactory cortex)
- dominant hemisphere language centres
- Posterior cerebral artery
- visual cortex
- hippocampus (long term memory)
- thalamus
- hypothalamus
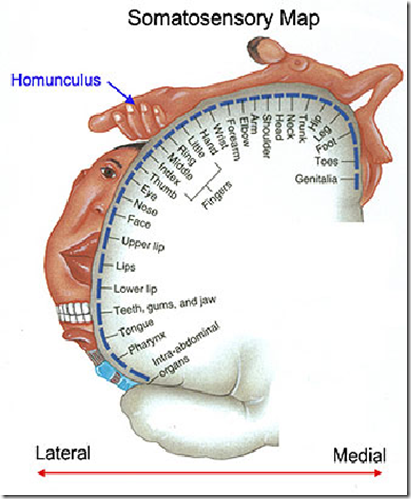
Somatosensory map with superimposed homunculus
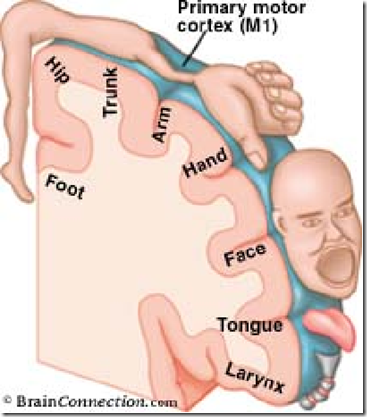
Motor map with superimposed homunculus
_____________________________________________________________________
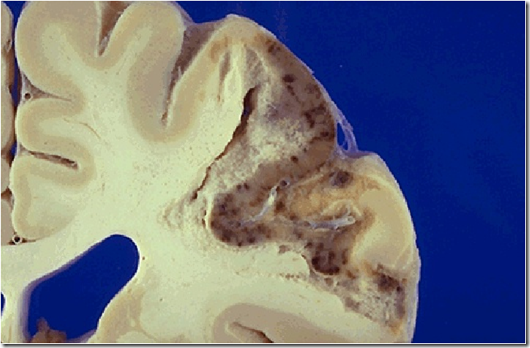
Stroke: Cerebral infarction
Pathogenesis
- lack of blood supply
- causes ischaemia –> resulting in tissue hypoxia
- Brain requires high oxygen supply
- brain tissue dies
- cerebral infarction
Causes of infarction
- Narrowing of blood vessels by atheromatous plaques
- results in decreased blood supply
- infarction
- Embolism
- more common than atheromatous narrowing
- embolism from
- vegetation of heart valve
- atheroma in aorta
- atheroma in cerebral circulation
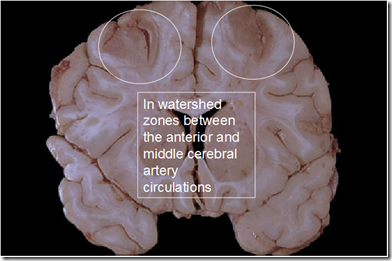
- Hypotension
- decreased blood flow in boundary zones (watershed regions) of the cerebral circulation
- (picture) above
- Liquefactive (colliquative) necrosis
- focal bacteria/fungal infection
- tissue digested by hydrolytic enzymes
- resulting in soft, circumscribed lesion
- consisting of pus and fluid remains of necrotic tissue
- after removal of cell debris by WBC, fluid filled space is left – abscess formation
- apopleptic cyst formation
- focal bacteria/fungal infection
Types of ischaemic stroke
- Total anterior circulation infarct (TACI)
- occlusion of internal carotid or MCA on one side
- Clinical features
- Drowsy/unconscious
- Complete hemiparesis
- Dysphasia (L) or neglect (R>L)
- Incontinence
- Hemianopia and deviation of eyes to side of stroke
- Poor prognosis
- Partial anterior circulation infarct (PACI)
- smaller wedge shaped infarct variable signs, less severe
- Clinical features
- Good recovery
- Likely to have further stroke
- Lacunar stroke (LACI)
- small discrete infarcts, often multiple
- associated with hypertension
- Posterior circulation infarct (POCI)
- vertebrobasilar infarction
- Brainstem damage
- so mortality high
- but good functional recovery if survive
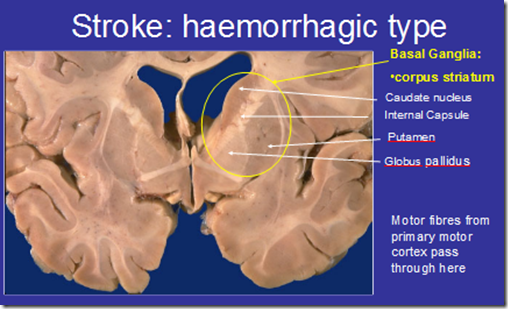
Types of haemorrhagic stroke
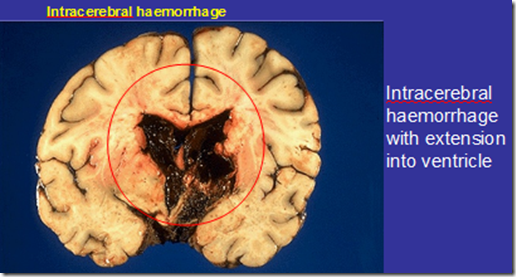
- Intracerebral Haemorrhage
- Microaneurysm formation in hypertensive patients
- Aneurysm forms on the penetrating vessels in the basal ganglia and internal capsule
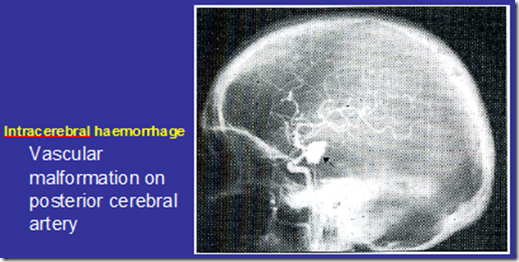
- Vascular malformation
- Haemorrhage into tumours
- Microaneurysm formation in hypertensive patients
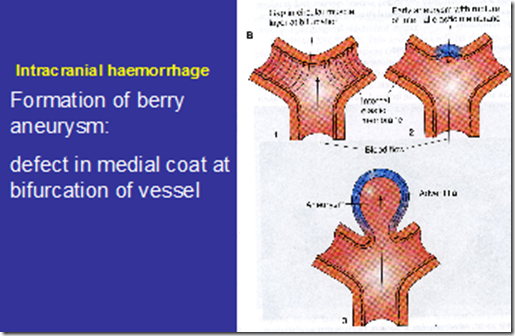
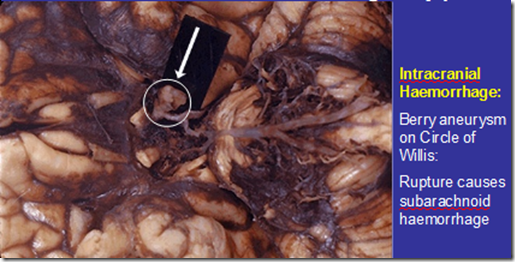
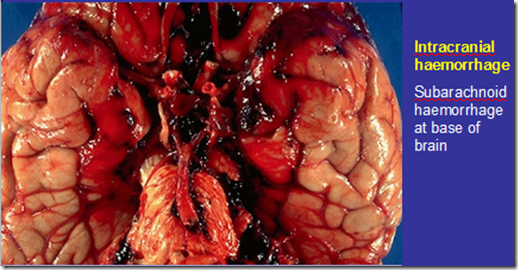
- Intracranial Haemorrhage
- Subarachnoid haemorrhage
- Caused by rupture of saccular (berry) aneurysm
- Sites of aneurysm formation on the Circle of Willis
- Defect in the middle layer at bifurcation of vessel
- 1-2% adult population
- 10-15% multiple
- women > men
- ‘congenital’
- Subarachnoid haemorrhage
_____________________________________________________________________
Transient Ischaemic Attack
- Known as mini strokes
- Pathogenesis
- change in the blood supply to a particular area of the brain
- resulting in brief neurologic dysfunction that persists, by definition, for less than 24 hours.
- If symptoms persist longer, then it is categorized as a stroke
- A cerebral infarct that lasts longer than 24 hours, but less than 72 hours is termed a reversible ischaemic neurologic deficit (RIND)
- change in the blood supply to a particular area of the brain
- Symptoms
- Temporary loss of vision
- Typically amaurosis fugax
- Amaurosis fugax is loss of vision in one eye due to a temporary lack of blood flow to the retinal
- artery
- Typically amaurosis fugax
- Dysphasia/aphasia weakness
- Weakness on one side of the body
- Numbness or tingling (paraesthesia)
- usually on one side of the body.
- Impairment of consciousness
- very uncommon
- Dizziness, lack of coordination or poor balance
- may vary in severity
- Temporary loss of vision
- Symptoms of a TIA are short lived and usually last a few seconds to a few minutes and most symptoms disappear within 60 minutes.
- Some individuals may have a lingering feeling that something odd happened to the body
Vertebro-basillar insufficiency
- Known as ‘hair saloon stroke’
- a type of transient ischaemic attack
- resolves within 24 hours
- Pathogenesis
- Hyperextending the neck can damage an artery
- Tearing of the artery lining
- blood starts flowing between layers of tissue and that can cause blood clots to start building up, leading to a stroke
- decreased blood flow in the posterior circulation of the brain
- medulla
- cerebellum
- pons
- midbrain
- thalamus
- occipital cortex
- Symptoms
- vertigo
- diplopia







I am very. interested