The arterial system is not very distensible (if distensible, then BP can be easily maintained when there is increase in volume), therefore arterial blood volume ∞ arterial blood pressure.
Determinants of arterial BP
- Cardiac Output (CO)
- Total Peripheral Resistance (TPR)
Therefore, BP = CO x TPR
Scenario
Effect of increase in blood volume towards blood pressure
- Cardiac Output , CO = HR x SV
- Increase in blood volume à increase in end diastolic volume à heart contract with greater force (Starling’s law) à Increase cardiac output à increase BP
- Veins are very distensible, therefore at least 60% of circulating blood volume is actually in the systemic veins.
- Increase in venous return à increase venous pressure (from increase in blood volume & venoconstriction)
Maintenance of blood volume
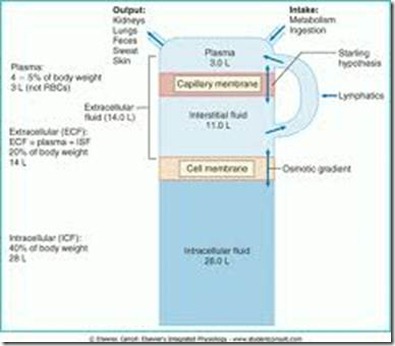
The circulating blood is composed of blood cells and plasma (55%). Plasma is composed of solids & water (90%). Therefore, to maintain blood volume, this water should stay in the intravascular (inside vessels) space.
However, as water moves along an osmotic gradient in event of dehydration, water moves from the circulating blood into the interstitial space, therefore blood volume will drop.
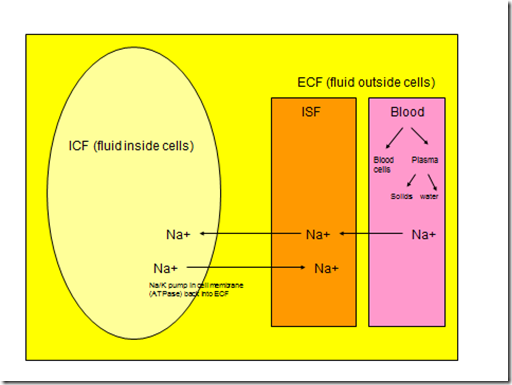
- Because of the Na/K pump, Na+ stays in the ECF
- Water moves along osmotic gradient, therefore wherever Na+ goes, water follows
- Therefore, Na+ is the backbone of ECF volume/blood volume
- Which is regulated by renal handling of Na+ (control Na* excretion and retention)
In normal healthy people,
- Increase in ECF volume does not increase Arterial BP.
- Why? Kidney is capable of maintaining Na+ balance. Excess Na+ and water will be excreted by the kidney.
- Renal handling of Na+ : mainly for regulation of blood volume & BP
- Renal handling of water: mainly for regulation of plasma osmolality
Blood pressure regulation/homeostasis
Short term regulation (within seconds)
- Neural
- Baroreceptor reflex
- Chemoreceptor reflex
- CNS Ischaemic response
Intermediate (within hours)
- Endocrine (catecholamines)
Long term regulation (within hours)
- Renal system
- Physical: by variation of Glomerular filtration pressure (GFR)
- Pressure diuresis (urine)
- Increase ECF Volume –> increase BP –> Increase renal perfusion pressure –> increase blood flow into glomerular capillaries –> increase hydrostatic pressure in glomerular capillaries -> increase GFR (more than increase in tubular absorption) –> increase urine formation
- Increase BP –> increase baroceptor reflex –> decrease sympathetic tone –> afferent & efferent arteriolar dilation (decrease vasoconstriction) –> increase blood flow into glomerular capillaries
- Pressure natriuresis (sodium)
- Increase urinary excretion of sodium
- Increase GFR –> increase amount of Na+ filtered (more than increase tubular reabsorption of Na+) –> Increase urinary Na+ excretion
- Amount Na+ filtered = GFR x plasma concentration of Na+
- Decreased blood volume & BP à decreased glomerular capillary pressure à decreased glomerular filtration rate
- Oliguria: decreased urine formation
- Anuria: renal shutdown – no urine formation
- Kidney conserves ECF volume
- Pressure diuresis (urine)
- Physical: by variation of Glomerular filtration pressure (GFR)
- Hormonal: by secretion of renin (Renin-angiotensin-aldoesterone system)
- 3 functions:
- Regulate blood volume
- By adjusting Na+ reabsorption)
- Regulate BP
- By vascular & volume effects
- Regulates plasma K+
- Regulate blood volume
- Source & control of renin : Juxtaglomerular apparatus (JA) consists of –
- Afferent arteriole (JG cells) – modified smooth muscle cells
- DCT (macula densa)
- Intervening Lacis cells
- Stimulus
- Renal sympathetic nerve activity
- stimulates renin secretion from granular cells
- Fall in systemic BP
- –> less pressure on afferent arteriole (JG cells) –> decrease stretch of afferent arteriole (intrarenal baroreceptor) –> stimulate release of renin
- Decrease transport of Na+ & Cl- across macula densa in DCT
- –> decrease NaCl to tubules –> macula densa secrete chemicals into ISF –> act on JG cells –> secrete renin
- Prostacyclin (intrarenal hormone)
- Renal sympathetic nerve activity
- 3 functions:
For the process of activation of the RAAS & its effects, read up from endocrine notes.
Angiotensin 2
Intrarenal actions
- Contraction of mesangial cells in glomerulus
- Decrease GFR
- Contraction of afferent & efferent arterioles
- Decrease RPF
- Increase GFR
- Since the effect on efferent arteriole is greater than afferent arteriole, the inflow decreases, outflow decreases more. Blood trapped in glomerullar capillary will increase GFR eventhough renal plasma pressure is low (no where else to go, slight pressure act as hydrostatic pressure instead of pressure for flow out of glomerulus)
- Increased Na+ reabsorption
- In the proximal tubule
Net effect on GFR — increased or maintained
Renal hypertension
Renal disease constricts the renal artery (renal artery stenosis) and decreases blood to afferent arteriole. RAA system will be activated from the decrease in renal pressure, hence systemic BP will increase as a compensation.
Hypertension can be divided into:
· Essential hypertension: no known cause
· Secondary hypertension: known cause (eg renal, endocrine)
Renal hypertension can be divided into:
- Renal parenchymal hypertension
- Chronic kidney disease
- Less nephron –> decreased GFR
- Chronic kidney disease
- Renovascular hypertension (see 1K1C model)
- Renal artery stenosis
- Atherosclerosis (most common in older patients)
- Fibromuscular dysplasia (young women)
- Renal artery stenosis
Hypertension in nephritic patients
The kidneys normally produce vasodilator prostaglandins (PGA, PGE) locally. In nephritic patients, these vasodilators is not produced, therefore there will be renal artery constriction and hence the BP rises.
High renin hypertension
When there is renal ischaemia, for some reason blood cannot reach the kidney, there will be renin production to increase the systemic blood pressure so that blood can enter the kidney. However, failure for blood to reach kidney even with renin, will cause a positive feedback whereby more renin will be produced due to the ischaemia, and therefore will cause overactivity of RAAS.
Low renin hypertension
When there is volume overload, and the kidney cannot excrete Na+, the excess water will be retained. Hence blood volume will be constantly high.
The renal pressure will be high, therefore renin will not be produced.
Kidney failure
If the kidney loses it’s function, the patients will become hypertensive. Therefore, chronic kidney disease is the most common cause of secondary hypertension. However, if this is so, hypertension can be relieved with hemodialysis and ultrafiltration.
From this graph, when the curve shifts to the right in impaired pressure natriuresis, the equilibrium point shifts and the mean arterial pressure is elevated. Hence, hypertension.
In this case, natriuresis is normal, however, if salt intake is increase, therefore the concentration increases, and a new equilibrium point is plotted. The blood pressure is increased and hence hypertension. This is also known as ‘salt sensitivity’.
Physiologically, the concentration is higher, therefore the osmotic pull of water is stronger than the hydrostatic push. Excess water cannot be excreted, therefore the systemic blood pressure cannot be reduced.
1K1C model – One kidney Goldblatt hypertension
When the clip is placed on the renal artery, a renal artery stenosis is produced. Therefore, decrease in blood entering the kidney will cause a extreme decrease in distal renal artery pressure, whereby it will stimulate high renin secretion for compensation. The systemic blood pressure will increase dramatically. Once the clip is released, renin secretion falls and the blood pressure decreases steeply back to normal.
This phenomenon can be used to describe the pathophysiology of these diseases (one kidney hypertension)
- Renal artery stenosis (in a singularly functioning kidney, 1 kidney)
- Bilateral renal artery stenosis (both kidenys)
- Aortic coarctation
- Decreases perfusion in both kidneys (which begins at a higher level, and affects all the other organs as well. But primarily the kidneys as they receive 90% of the blood)
2K1C model – Two kidney Goldblatt hypertension
This experiment is performed on an animal with 2 functioning kidneys, but a clip is placed on only 1 of the renal artery.
This phenomenon can be used to describe the pathophysiology of these diseases ( two kidney hypertension)
- Unilateral renal artery stenosis
- Affects only 1 of the 2 kidneys
- Unilateral atherosclerotic renal artery disease
- Tumour compressing one renal artery
- Pheochromocytoma
Renal changes in ‘essential hypertension’
As we’ve discussed how renal diseases can cause secondary hypertension, now we’ll discuss about how primary/essential hypertension can cause changes to the kidney.
- Reduced renal perfusion
- RBF less than 50% in later stages
- High BP maintains almost normal GFR
- But falls in later stages
- Salt and water retention
- Renal failure
- But falls in later stages
- Activation of RAAS
- Salt & water retention
Hypertensive nephropathy (hypertensive renal disease)
Based on 2 pathophysiologic mechanisms
- Glomerular ischaemia
- Chronic hypertension -> narrowing of preglomerular arteries & arterioles (arteriosclerosis) why? -> reduction in glomerular & tubular blood flow –> ischaemia –> Atrophic nephron –> impaired nephron function –> impaired renal function
- Glomerular hyperfiltration
- Hypertension causes some glomeruli to become sclerotic
- The remaining nephron undergo compensatory vasodilation of the preglomerular arterioles –> increase in renal blood flow –> glomerular hyperfiltration –> progressive glomerular sclerosis & tubular damage –> dilated atrophic
nephrons –> impaired nephron function & a decrease in the no of functioning nephrons –> impaired renal function.
Salt sensitivity (in essential hypertension)
- Salt-sensitive hypertension
- BP falls with salt restriction
- Salt-insensitive hypertension
- BP does not respond to salt restriction
* in response to therapeutic attempt by reducing salt intake



very nice information
Your notes is so beneficial