Micturition: Process by which urinary bladder empties. It is a complex act involving both autonomic & somatic nerve pathways & several reflexes that can be either inhibited or facilitated by higher centers in the brain.
Micturition involves 2 important steps:
- Bladder fills progressively
- tension in bladder wall increases
- Initiates a nervous reflex
- micturition reflex: empties the bladder/causes conscious desire to urinate
- Autonomic spinal cord reflex, inhibited/facilitated by centers in brain stem & cerebral cortex
Stages
- Transport of urine to bladder
- Filling phase
- Voiding phase
_____________________________________________________________________
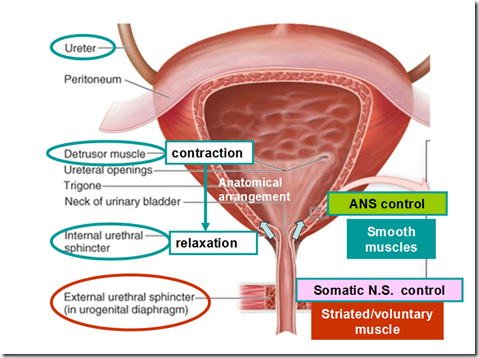
Urinary Bladder
- Smooth muscle chamber
- detrusor muscle
- arranged in spiral, longitudinal & circular bundles
- contraction can increase pressure in the bladder to 40-60 mmHg
- ureters run obliquely through the detrusor muscle and then passes another 1-2 cm beneath the mucosa before emptying into the bladder
- detrusor muscle
- Bladder trigone
- small triangular area in the posterior wall of bladder
- 2 ureters enter the bladder at the uppermost angles of the trigone
- inner lining of the bladder at trigone is smooth
- the rest is folded to form rugae
- Internal & external sphincters
- internal sphincter – formed from detrussor muscle at bladder neck (posterior urethra) with elastic tissue
- smooth muscle
- normal tone of internal sphincter prevents emptying of bladder
- external sphincter – formed from a layer of skeletal muscle
- skeletal muscle
- under voluntary control of the nervous system
- internal sphincter – formed from detrussor muscle at bladder neck (posterior urethra) with elastic tissue
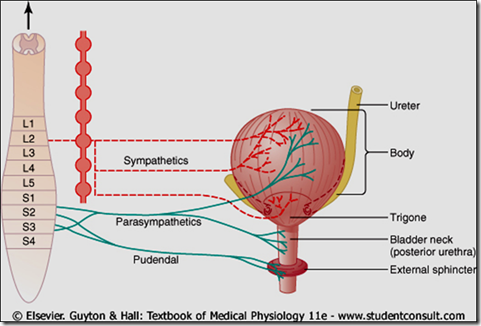
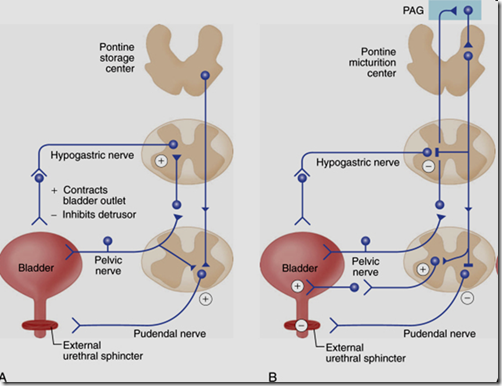
Bladder nerves
Somatic
- Pudental nerves (S2,S3,S4)
- motor & sensory fibres
- External urethral sphincter
Sympathetic
- Hypogastric nerves (L1,L2,L3)
- motor & sensory fibres
- Bladder wall relaxation
- Internal sphincter contraction
Parasympathetic
- Pelvic nerves (S2,S3,S4)
- motor & sensory fibres
- Bladder wall contraction
- Internal sphincter relaxation
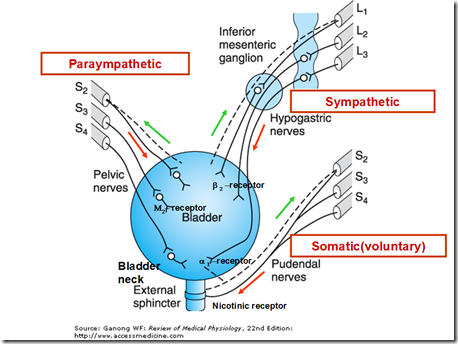
Actions of bladder nerves
- Sympathetic postganglionic neurons release noradrenaline (NA)
- activates b3 adrenergic receptors
- relax bladder smooth muscle
- activates a1 adrenergic receptors
- contract urethral smooth muscle (internal sphincter?)
- activates b3 adrenergic receptors
- Parasympathetic postganglionic axons in pelvic nerve release acetylcholine (ACh)
- stimulate M3 muscarinic receptors in the bladder smooth muscle
- bladder contraction
- stimulate M3 muscarinic receptors in the bladder smooth muscle
- Somatic axons in the pudendal nerve release ACh
- activates nicotinic cholinergic receptors (neuromuscular junction)
- contract external sphincter striated muscle
- activates nicotinic cholinergic receptors (neuromuscular junction)
Bladder nerve supply
- Sensory fibers in pelvic nerves sense the degree of stretch in the bladder wall
- Stretch signals from posterior urethra are more powerful in initiating the micturition reflex
- Motor nerves transmitted in the pelvic nerves terminate on ganglion cells located in the wall of the bladder
- postganglionic nerves innervate the detrusor muscle
- Pudendal nerves carry skeletal motor fibers to external sphincter
- Control the voluntary skeletal muscle sphincter
- Sympathetic innervation from the sympathetic chain through the hypogastric nerves
- Sympathetic innervation mainly to blood vessels
- Important in the sensation of fullness/pain
- lower abdomen
- In males – mediate the contraction of the bladder muscle (internal sphincter)
- that prevents semen from entering the bladder during ejaculation
- retrograde ejaculation
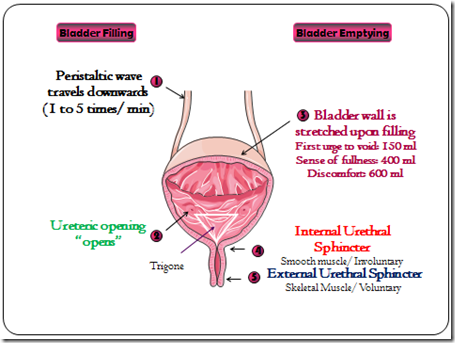
Transport of urine into the bladder
- Urine flow out of collecting duct
- No change in composition during its flow in renal calyces & ureter
- Peristaltic contractions in ureter
- initiated by pacemaker activity in renal calyces
- calyces contain specialized smooth muscle cells that generate spontaneous pacemaker potentials
- unstable resting potential
- peristaltic waves sweep down the ureters
- frequency 1 every 10 seconds – 2/3 minutes
- stimulated by parasympathetic nerves
- inhibited by sympathethic nerves
- forces urine into the bladder
- normal tone of detrusor muscle prevents backflow of urine into ureter
Problems that can occur
- Vesicoureteral Reflux
- Urine of the bladder is propelled backward into the ureter during contraction of bla
dder - Enlargement of ureters
- Urine of the bladder is propelled backward into the ureter during contraction of bla
- Ureterorenal Reflex
- Blockage of ureter by ureteral stones
- causes reflex constriction of ureter
- increased pain sensation
- sympathetic reflex to constrict renal arterioles
- to decrease the renal output/urine formation
- Prevents excessive flow of fluid into renal pelvic of a kidney with a blocked ureter
- Blockage of ureter by ureteral stones
Bladder filling & emptying
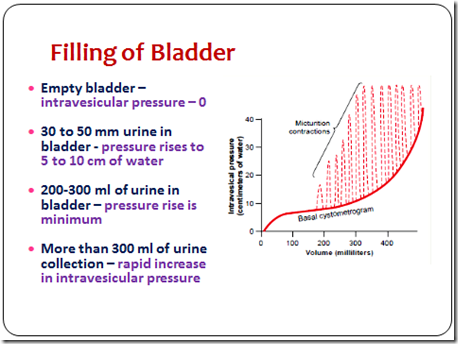
Bladder filling
- Empty bladder
- 0 – intravesicular pressure
- 30-50 ml urine in bladder
- pressure: 5-10cm of water
- 200-300 ml urine in bladder
- pressure rise minimum
- more than 300ml urine
- rapid increase in pressure
First sensation of bladder filling is experienced at a volume of 100 – 150 ml in an adult. Then the 1st desire to void/urinate is when the bladder contains about 150-250 ml of urine. A person becomes uncomfortably aware of a full bladder when the volume is 350-400 ml. The volume of urine that normally initiates a reflex contraction is about 300-400 ml. An increase in volume to 700 ml creates pain and loss of control!
Cystometrogram
- A plot of intravesical pressure vs volume of fluid in the bladder
- Ia – initial slight rise in pressure
- Ib – long nearly flat segment
- Law of Laplace
- Pressure in a spherical viscus is equal to twice the wall tension divided by the radius
- P = 2T / r
- Due to its ability to stretch, T (Tension) increase will cause r (radius) increase as well, therefore P (pressure) will not increase much.
- This gives us the ability to fill the bladder beyond 300ml
- II – sudden sharp rise in pressure ( micturition reflex triggered)
Micturition Reflex
A single complete cycle of:
- Progressive & rapid increase of pressure
- A period of sustained pressure
- Return of the pressure to the basal tone of the bladder
Receptor
- Sensory stretch receptors in bladder wall
- receptors in the posterior urethra are highly sensitive to stretch when the area begins to fill with urine at the higher bladder pressures
Afferents
- through pelvic nerves
Center
- Spinal cord
- Pons
- Medulla
- Hypothalamus
- Cortex
Efferents
- through pelvic nerves
Effector organ
- Detrusor muscle
- Internal & external sphincters
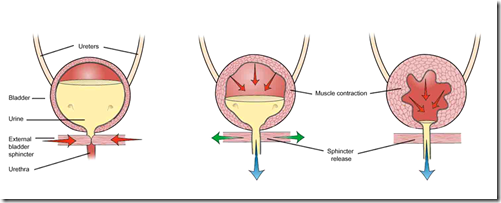
Micturition Reflex – Process
- Sensory signals from the bladder stretch receptors sent to spinal cord
- Parasympathetic efferent fibers discharge
- produce ‘micturition contractions’
- initially die out immediately, but with increasing pressure in bladder these become stronger & last longer & more frequently
- Reflex will not empty the bladder always
- may become inhibited for a period of few minutes to one hour before another reflex occurs
- ‘self-regenerative’
- Urination occur when
- powerful micturition reflex
- cortical inhibition removed
- relax external sphincter
- relaxation of pelvic floor muscles
- Increase intra-abdominal pressure
- by contracting abdominal muscles
- Relaxation of internal & external sphincters
Higher Centers for Micturition
The higer centers keep the micturition reflex partially inhibited, except when desired/during urination. It can prevent micturition, even if the micturition reflex occurs, by tonic contractions of the external sphincter until it is convenient to urinate. When it is time to urinate, the cortical centers can facilitate the sacral micturition centers to help initiate the external urinary sphincter so that urination can occur.
Cerebral lesions (like tumors, Parkinsons, vascular accident) are known to affect the perception of bladder sensation and can result in voiding dysfunction (loss of control/dribbling)
- Facilitatory areas
- Pons
- Posterior hypothalamus
- Inhibitory areas
- Cerebral cortex
- Midbrain
Micturition in young children
- micturition is purely reflex
- occurs whenever the bladder is sufficiently distended
- myelination not complete
- occurs whenever the bladder is sufficiently distended
- About 2 1/2 years old, it begins to come under cortical control
- About 3 years old, complete control is achieved
- cortex takes over control
- Female after child-birth
- weakened pelvic floor muscle
- loss of bladder control causing urine leakage
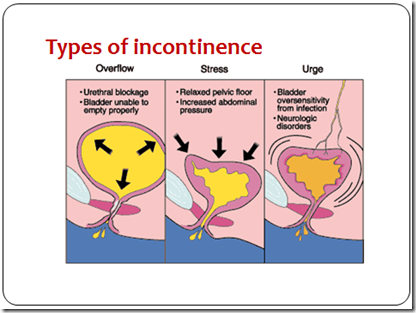
- Sign & symptoms
- Frequency – urinate more than 7 times a day / more than 2 times at night
- Urgency – desire to urinate with a volume of less than 50ml
- Dysuria – pain during micturition
- May result from
- Hyperactive micturition reflex
- due to irritation (urge incontinence)
- Effort/exertion/coughing/sneezing
- pelvic floor weakness (stress incontinence)
- Overdistension of bladder
- urethral obstruction (overflow incontinence)
- Hyperactive micturition reflex
- Neural causes of incontinence
- Atonic bladder
- Bladder loss the tone
- Cause: sensory nerve fibers (afferent) from bladder to spinal cord are damaged
- crush injury to the sacral region of the spinal cord, tumours, tabes dorsalis
- intact efferent fibers
- all reflex contractions of bladder lost
- Bladder becomes distended, thin-walled and hypotonic
- The bladder fills to capacity and overflows a few drops at a time through the urethra
- overflow incontinence
- Denervation/Hyperactive bladder
- Cause:
- tumors of cauda equina / filum terminale
- Bladder flacid & distended
- Gradually, muscle of the ‘decentralised bladder’ becomes active and shows many contraction waves
- Dribbling of urine out of urethra
- Bladder becomes shrunken & bladder wall hypertrophied
- denervation hypersensitivity
- increase tone
- hyperthophy
- Cause:
- Automatic bladder
- Cause: spinal cord damage above sacral region
- Higher center control is loss (voluntary control loss)
- Sacral micturition reflex centers are intact
- Suppression of micturition reflex during spinal shock due to loss of facilitatory impulses from brain
- reflex returns after spinal shock
- Bladder becomes overfilled , can’t urinate voluntarily
- urine dribbles through sphincters
- overflow incontinence
- urine dribbles through sphincters
- Cause: spinal cord damage above sacral region
- Uninhibited Neurogenic Bladder
- Cause: damage to brain/spinal cord that control inhibitory signals for micturition
- Frequent and uncontrolled micturition
- continuous facilitatory signals to bladder
- even a small quantity of urine in bladder initiate powerful micturition reflex and empties the bladder
- Atonic bladder
- Age-related changes
- Frequency of involuntary bladder contraction increases
- Total bladder capacity decreases
- voiding urge at lower volumes
- Bladder contractility decreases
- increased postvoid residuals
- increased sensation of urgency/fullness
- Increase incidence of nocturia
- night awakenings
- Women
- menopausal estrogen decline
- urogenital atrophy
- decrease in sensitivity of receptors in the internal sphincter – less tone
- urogenital atrophy
- menopausal estrogen decline
- Men
- Prostatic hypertrohpy
- increased urethral resistance
- varying degrees of urethral obstruction
- higher frequency of urination, however unable to urinate much
- stream of urine not smooth
- Prostatic hypertrohpy




Do you have any references for the information you have supplied?
Kind regards,
Claire