Osteoarthritis (OA)
- General
- Degenerative joint disease
- No known cure
- Therapeutic objectives
- reduce pain
- improve joint mobility
- limit functional impairment
- Management
- Patient education
- lose weight
- lessen burden of weight-bearing joints
- exercise
- Non-medicinal & rebilitative
- exercises
- range-of-motion
- muscle-strengthening
- braces, orthotics, assistive devices
- appropriate footwear
- occupational therapy
- Pharmacotherapy
- Oral
- NSAIDs
- COX2 selective inhibitors
- glucosamine
- Intra-articular injection
- Glucocorticoids
- Hyaluronic acid
- Topical
- NSAIDs
- Surgery
Rheumatoid arthritis (RA)
- Therapeutic objectives
- Pain relief
- Reduce inflammation
- Control disease activity
- prevent/slow joint damage
- prevent loss of function
- improve quality of life
- correct/compensate mechanical & structural abnormalities by assistive devices
- Induce a remission (if possible)
- a state of absence of chronic disease
- Therapeutic measures
- Pharmacologic
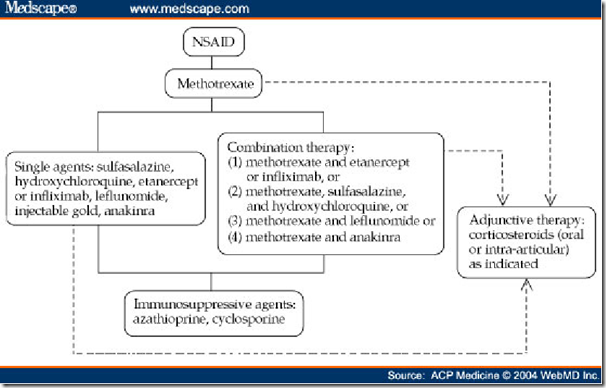
- NSAIDs
- reduce joint pain & swelling
- pharmacologic actions
- analgesic
- antipyretic
- anti-inflammatory
- Glucocorticoids
- Drugs that suppress the rheumatoid disease process
- Disease-modifying anti rheumatic drug (DMARDs)
- Biologic response modifiers
_____________________________________________________________
NSAIDs
- pharmacologic actions
- analgesic
- antipyretic
- anti-inflammatory
- pharmacology
- Inhibits COX-1 & COX-2
- reduce production of prostaglandins
- analgesic, antipyretic, anti-inflammatory
- Side effects
- Inhibition of COX-1 in gastric epithelial cells
- gastic ulcer/bleeding
- Inhibition of COX-1 & 2 in kidney
- interfere with regulation of renal blood flow
- nephrotoxicity
- Inhibit platelet TXA2 formation
- prevent platelet aggregation
- Increased cardiovascular thrombotic risk
- but can be used as anti-thrombosis
- Classification (based on potency)
- Moderate potency
- Fenamates
- mefenamic acid
- Propionic acids
- naproxen
- ibuprofen
- ketoprofen
- Paraaminophenol derivative
- acetaminophen
- paracetamol
- High potency
- Salicylates
- aspirin
- diflunisal
- Acetic acids & derivatives
- indomethacin
- sulindac
- etodolac
- diclofenac sodium
- Oxicams
- piroxicam
- meloxicam
- Pyrazolones
- phenylbutazone
- COX-2 selective inhibitor
- Celecoxib
- valdecoxib
- meloxicam
- Therapeutic uses
- Analgesic, Antipyretic, Anti-inflammatory
- Closure of patent ductus arteriosus
- in neonates
- indomethacin
- Dysmenorrhea
- COX2 inhibitors
- Systemic mastocytosis
- due to prostaglandin released from mast cells
- induce vasodilation & hypotension
- prevented by NSAIDs
- Bartter’s syndrome
- excessive productionof renal prostaglandins
- Prevention of colon cancer
- Contraindication
- Aspirin in children <16 yo
- risk of Reye’s syndrome
- Adverse effects
- Gastric/intestinal ulceration
- Increased bleeding time
- prevent formation of platelet-TXA2
- Renal dysfunction
- decrease RBF & GFR
- renal insufficiency
- hyperkalemia
- proteinuria
- Salt & water retention
- oedema
- hypertensive
- antagonize the action of anti-hypertensives
- Hypersensitivity
- rashes
- urticaria
- vasomotor rhinitis
- angioneurotic oedema
- bronchial asthma (aspirin)
- Abnormal liver function tests
- During pregnancy
- prolongation of gestation
- delay labour
- early closure of ductus arteriosus
- fetal distress
- Choice of NSAIDs
- based on side effects
- risks of upper GI side effects
- Phenylbutazone
- highest risk
- Ibuprofen
- lowest risk
- do not use more than 1 oral NSAIDs simultaneously
- COX-2 inhibitors (NSAIDs)
- as effective as older NSAIDs
- lower incidence of upper GI ulceration
- for patients with high risk of GI ulceration
- no difference in bleeding
- more expensive
- Higher rate of thrombotic events
- non-fatal myocardial infarction
- non-fatal strokes
- Acetaminophen & paracetamol
- Inhibits COX-3
- analgesic & antiypyretic effects
- metabolised in liver
- through glucoronic acid conjugation
- small % undergo cytochrome P450 mediated N-hydroxylation
- forming highly reactive intermediate
- associated with hepatotoxicity in large doses
- half life of 2 hours
- no risk of upper GI ulceration & bleeding
- effective for osteoarthritis
- less for inflammatory arthritis
_____________
________________________________________________________
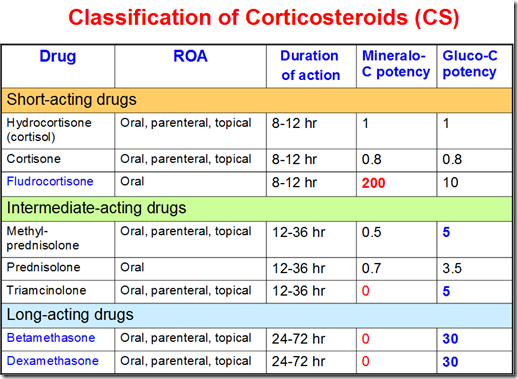
Glucocorticoids
- RA
- low-dose oral glucocorticoids
- relieve symptoms
- slows rate of joint damage
- Local injection
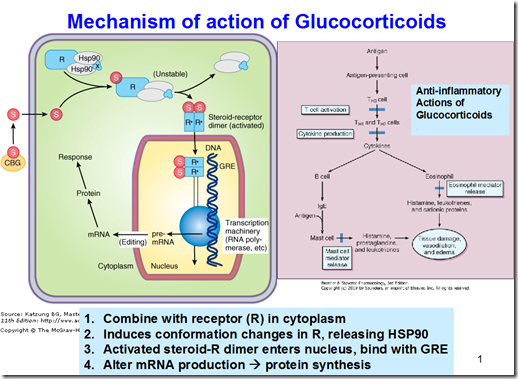
- Pharmacological actions
- anti-inflammatory & immunosuppression
- suppress activation of T-cells, APC, macrophages
- by cytokines
- suppress production of cytokines
- block PLA2
- decrease release of chemical mediators of inflammation (from mast cells, eosinophils etc)
- histamine
- prostaglandins
- leukotrienes
- PAF
- stabilize lisosomal membranes of neutrophils
- prevent release of catabolic enzymes
- acid phosphatase
- increase synthesis of lipocortin
- inhibit PLA
- decrease prostacyclin
- decrease capillary permeability
- promote vasoconstriction
- reduce inflammation
- Increase serum glucose
- increase insulin secretion
- stimulate hormone sensitive lipase
- lipolysis
- increase insulin secretion stimulate lipogenesis, inhibit lipolysis
- fat deposition on trunk
- Cushing’s disease
- Replacement therapy in adrenal insufficiency
- Anti-inflammatory & immunosuppressive
- Allergy
- bronchial asthma
- RA, OA
- organ transplantation
- ARDS
- malignancies
- cerebral oedema
- nephrotic syndrome
- eye, skin disease
- IBD
- Check & monitor for:
- hyperglycemia
- glaucoma
- cataract
- hidden infections
- BP
- hypokalemia
- peptic ulcer
- osteoporosis
- Patietns with
- Diabetes mellitus
- Glaucoma
- Peptic ulcer disease
- hypertension
- with heart failure
- TB
- Varicella virus infection
- Psychosis
- Osteoporosis
- Cushing’s syndrome
- Adrenal suppression
- avoid sudden withdrawal
- Immunosuppression
- infection
- Others
- osteoporosis
- hypertension
- weight gain
- fluid retention
- hyperglycemia
- cataracts
- glaucome
- skin fragility
- premature atherosclerosis
_____________________________________________________________________
Disease Modifying Anti-rheumatic Drugs (DMARDs)
- In RA
- reduce/prevent joint injury
- early use
- preserve joint integrity & function
- Advantages
- economic
- control symptoms in the long term
- Disadvantages
- no immediate analgesic effects
- slow action: 8-12 weeks
DMARDs Agents
- Methotrexate (MTX)
- MOA
- folic acid inhibitor
- inhibits
- lymphocyte proliferation
- production of cytokines
- rheumatoid factor
- Interferes with neutrophil chemotaxis
- reduces production of cytotoxins & free radicals
- that damage synovial membrane & bone
- effective in reducing signs & symptoms of RA
- Highest efficacy
- without excess toxicity on long term use
- Taken orally/subcutaneously
- Adverse effects
- Most serious (but rare)
- hepatic cirrchosis
- interstitial pneumonitis
- severe myelosuppression
- Stomatitis, Mild alopecia, GI upset
- related to folic acid antagonism
- management: give folic acid
- Contraindication
- patients with pre-existing
- liver disease
- hepatic dysfunction
- alcohol abuse
- Leflunomide
- MOA
- block intracellular enzyme
- needed for de novo pyrimidine synthesis
- Actions
- antiproliferative
- anti-inflammatory
- immunosuppressive
- As effective as methotrexate
- decrease signs & symptoms
- decrease joint damage
- Metabolism
- converted to active metabolite in GI wall & liver
- Onset of action
- relatively fast (1-2 months)
- sustained
- Adverse effects
- diarrhea
- rashes
- alopecia
- elevation of liver enzymes
- possible liver damage
- Potent teratogen
- discontinue & undergo cholestyramine washout before attempting conception
- Monitor blood count & hepatic function
- Sulfasalazine (SSZ)
- Metabolism
- reaches the colon
- splits into 2 components by bacteria
- important for action
- Onset of action
- as early as 1 month
- Action
- reduce
signs & symptoms of RA - slow/halt radiolographic progression
- Adverse effects
- hypersensitivity
- sulfa allergy
- mild GI upset
- mild cytopenia
- Monitor blood every 1-3 months
- Good alternative to methotrexate
- for patients with liver disease
- less toxic to liver
- Hydroxychloroquine
- MOA
- reduces chemotaxis & phagocytosis of polymorphs
- Onset
- slow
- Use for
- milder RA
- less effective than SSZ & MTX
- but less toxic & better tolerated
- Side effects
- ocular toxicity*
- maculopathy
- scotoma
- Monitor
- baseline & annual ophthalmologic assessments
- Stop therapy
- if any impairement of vision
- severe rash
- Sodium aurothiomalate (Gold therapy)
- Given Intramuscularly
- after injection, do CBC & urine test for protein
- Side effects
- skin rash
- stomatitis
- flushing
- hypotension
- tachycardia
_____________________________________________________________________
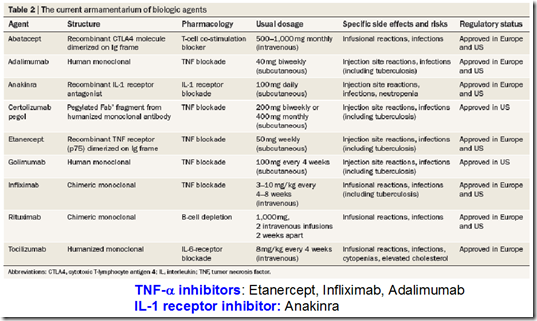
Biologic response modifiers
TNF-alpha blockers
- Etanercept
- recominant fusion protein (consist of)
- soluble human TNF-receptor
- human IgG1-Fc fragment
- MOA
- binds TNF-alpha in the circulation & in joint
- prevent interaction with cell surface TNFa receptors
- reduce TNF activity
- clears TNFa from circulation
- Used in combination with MTX
- if MTX alone not enough
- Onset
- 1-4 weeks
- Given subcutaneously
- Very expensive
- Infliximab/Adalimumab
- MOA
- Monoclonal antibody that binds TNFa
- with high affinity & specificity
- same mechanism as (above)
- Used in combination with MTX (same)
- Onset
- days – weeks
Adverse effects for TNFa blockers
- Injection site
- pain
- swelling
- itching
- Serious infections
- sepsis
- death
- Disseminated tuberculosis
- reactivation of latent disease
- screening for latent TB essential before treatment
- Lymphoma
- non-hodgkin’s lymphoma
- RA itself is a risk
- Do not use in patients with
- demyelinating disease
- congestive heart failure
Other drugs
- Anakinra
- recombinant
- non-glycosylated human IL-1Ra
- MOA
- inhibits binding of cytokine to IL-1 receptor
- Used with DMARDs
- Onset
- 2-4 weeks
- Given subcutaneously
- Side effects
- injection site reactions
- serious infections
- decreased white blood cell count
- lymphoma
- Combination of biologics not recommended
- risk of infections increased if combine with TNFa inhibitors
- Advantage
- no case of TB reported
- does not reactivate latent TB
- Abatacept
- MOA
- inhibits activation of T cells
- by blocking co-stimulatory signal
- Given alone/with DMARDs
- Side effects
- risk of infection
- URTI
- Rituximab
- MOA
- targets lymphocytes
- cause depletion of B cells
- Given IV
- Side effects
- rashes
- Advantage
- does not reactivate TB
- does not cause lymphoma
_____________________________________________________________________
Algorithm for Rheumatoid arthritis



If you have advanced arthritis and recommend that the relief operation for a while but does not replace painkillers such as hydrocodone. This medication should be taken to control and that can lead to addiction.